1 Diagnosis
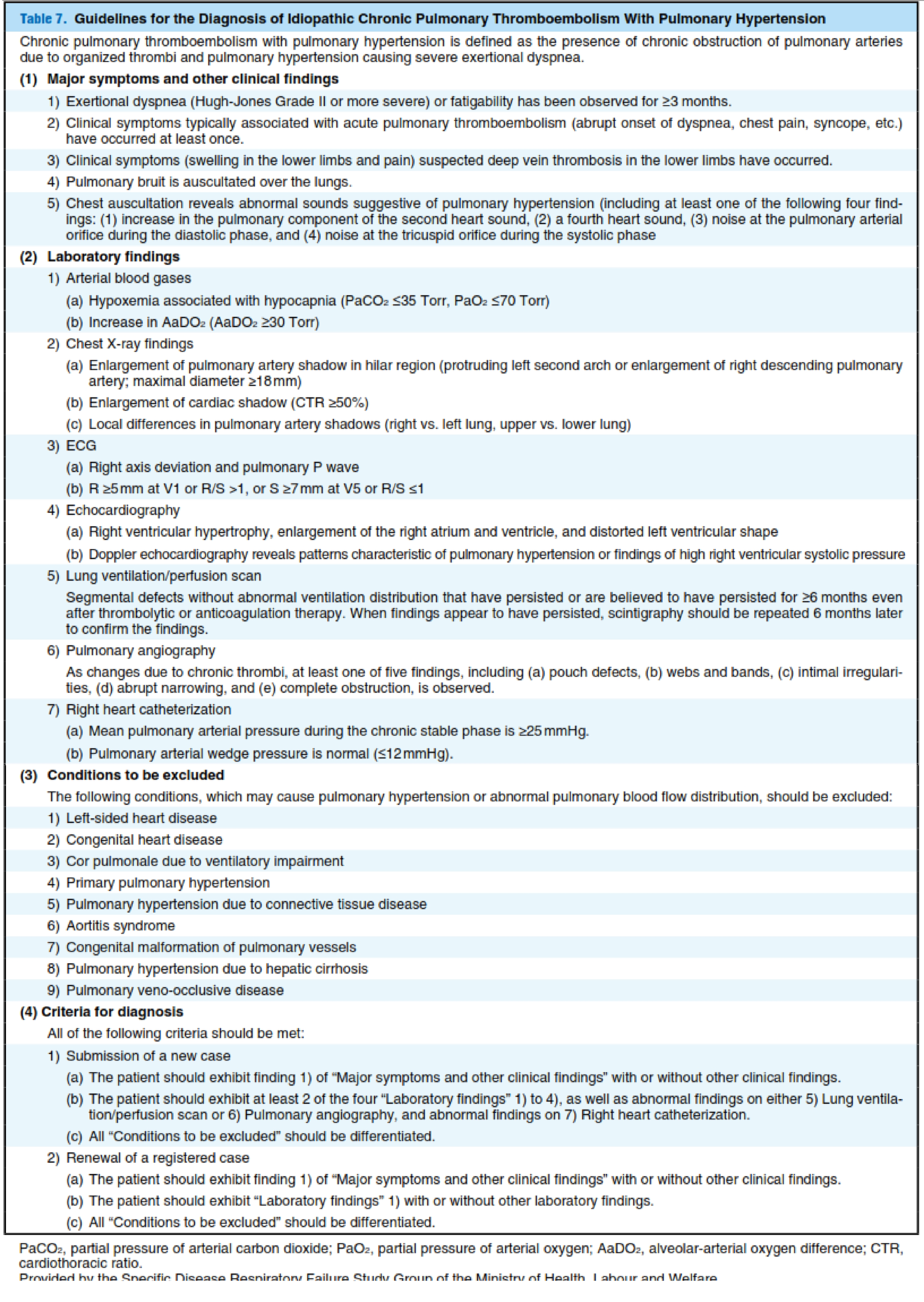
Diagnosis of idiopathic chronic PTE with PH (CTEPH) as a condition requiring treatment should be made according to the criteria for diagnosis provided by the Specific Disease Respiratory Failure Study Group of the MHLW (Table 7). CTEPH should be suspected in patients with exertional dys- pnea. Patients in whom CTEPH is suspected should be iden- tified based on the typical symptoms and clinical findings listed in Table 7.
Arterial blood gas analysis should be per- formed not only in patients with abnormal chest X-ray find- ings but also in those without remarkable X-ray findings. Patients with hypoxemia associated with hypocapnia should be assessed with ECG, echocardiography, and pulmonary function tests to exclude other cardiopulmonary diseases and to confirm the presence/absence of findings of right heart overload such as right ventricular enlargement and right ven- tricular hypertrophy. In making the diagnosis of CTEPH, physicians should confirm that (1) pulmonary ventilation/per- fusion scintigraphy has revealed maldistribution of pulmonary blood flow without abnormal ventilation distribution that has persisted for ≥6 months; or the patient exhibits at least one of the five typical findings of pulmonary artery angiog- raphy,ie, (a) pouch defects (the presence of round pouch- like shadows of thrombi that have been smoothed by blood flow, (b) webs and bands (band-like stenosis with pulmonary recanalization associated with organization of thrombi, (c) intimal irregularities, (d) abrupt narrowing, and (e) complete obstruction; and (2) right heart catheterization reveals normal pulmonary artery wedge pressure and a mean pulmonary arte- rial pressure of ≥25 mmHg. Cardiac catheterization is useful for measurement of pulmonary vascular resistance to deter- mine prognosis.
Although contrast CT (MSCT) has been reported to be useful in the diagnosis of CTEPH,pulmonary angiography is required to assess the condition of subsegmental arteries and to determine whether surgery is indicated.
2 Treatment
CTEPH is treated with medical and surgical therapy, and the results with current methods of PEA are excellent. Only a few reports have described catheter interventions for the treatment of CTEPH; use of them is not expected to become common in the future, if they are used at all.
(1) Medical Treatment
The pathophysiology of CTEPH includes PH due to occlu- sion of pulmonary arteries by organized thrombi, intractable right heart failure, and hypoxemia. Accordingly, surgical removal of organized thrombi (PEA) is the only radical treat- ment for CTEPH. However, PEA is limited to the treatment of central type of CTEPH. Patients with peripheral type of CTEPH, those with relatively mild CTEPH who do not need surgery, and those with CTEPH with persistent PH following surgery are treated with medical treatment.
In medical treatment, patients with CTEPH who are not indicated for surgery receive anticoagulants for the treatment of VTE, which is considered the cause of CTEPH, oxygen therapy for hypoxemia, pulmonary vasodilators for PH, and cardiotonics and diuretics for right heart failure, whenever necessary.
1. Anticoagulation Therapy
The prognosis of untreated CTEPH depends on pulmonary hemodynamics. It has been reported that even patients with mild CTEPH may exhibit exacerbation of pulmonary hemo- dynamics over time. Such exacerbation is believed to be caused by recurrent acute PTE, and to involve mechanisms of formation of thrombus in situ. Accordingly, life-long anti- coagulation therapy with warfarin is required for patients with CTEPH. Warfarin is often administered with a target INR of 1.5 to 2.5, which is also recommended for patients with acute PTE.
2) Thrombolytic Therapy
Patients with CTEPH may exhibit rapid progression of dis- ease. When levels of coagulation/fibrinolytic molecular markers such as D-dimer are high during disease progression, thrombolytic therapy may yield improvement. Physicians should be aware of this possibility.
3) Hypoxemia
Although there is no conclusive evidence for it, oxygen ther- apy is expected to improve both the QOL and prognosis of patients with CTEPH. In Japan, home oxygen therapy (HOT) for patients with PH including CTEPH is covered by the NHI.
4) Treatment of Right Heart Failure
The presence of clinically significant right heart failure is an important determinant of the prognosis in CTEPH. Patients with right heart failure who exhibit pleural effusion, hepa- tomegaly/abnormal hepatic function, thrombocytopenia, leg edema, or other typical signs/symptoms are treated with con- ventional regimens for heart failure including bed rest, restric- tion of water intake, diuretics, and oral cardiotonics. Patients in severe condition also require intravenous administration of catecholamines such as dopamine and dobutamine as well as milrinone.
5) Vasodilatation
Although use of classic vasodilators such as calcium blockers, nitrates, and angiotensin converting enzyme (ACE) inhibi- tors to treat CTEPH has been attempted, the efficacy of these drugs in patients with CTEPH has not been demonstrated. However, recent studies have evaluated the effects of bera- prost and epoprostenol,drugs indicated for pulmonary arterial hypertension, on CTEPH. Open-label studies and placebo-controlled studies of bosentanand sildenafil have revealed that these drugs may significantly improve pulmonary hemodynamics, six-minute walking distance, and brain natriuretic peptide (BNP) level, and so on. The efficacy of regimens combining these drugs has also been reported. However, use of these drugs for the treatment of CTEPH is currently not covered by NHI in Japan.
[Levels of Recommendations]
1. Anticoagulation therapy: Class IIa
2. Oxygen therapy/HOT: Class IIb
3. Vasodilatation for the treatment of PH: Class IIb
4. Cardiotonics and diuretics for right heart failure: Class IIb
Source "Guidelines for the Diagnosis, Treatment and Prevention of Pulmonary Thromboembolism and Deep Vein Thrombosis (JCS 2009)"
Duc Tin Surgical Clinic
Tin tức liên quan

Performance diagnostique de l’interféron gamma dans l’identification de l’origine tuberculeuse des pleurésies exsudatives

A Mixed Phenotype of Airway Wall Thickening and Emphysema Is Associated with Dyspnea and Hospitalization for Chronic Obstructive Pulmonary Disease.

Radiological Approach to Asthma and COPD-The Role of Computed Tomography.

Significant annual cost savings found with UrgoStart in UK and Germany

Thrombolex announces 510(k) clearance of Bashir catheter systems for thromboembolic disorders
Phone: (028) 3981 2678
Mobile: 0903 839 878 - 0909 384 389







