Background
Atrioventricular (AV) block occurs when atrial depolarizations fail to reach the ventricles or when atrial depolarization is conducted with a delay. Three degrees of AV block are recognized.
Atrioventricular (AV) block occurs when atrial depolarizations fail to reach the ventricles or when atrial depolarization is conducted with a delay. Three degrees of AV block are recognized.
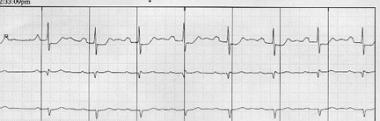
First-degree AV block consists of prolongation of the PR interval on the electrocardiogram (ECG) (>200 msec in adults and >160 msec in young children). The upper limit of the reference range for the PR interval is age-dependent in children. All atrial impulses reach the ventricles in first-degree AV block; however, conduction is delayed within the AV node (see the image below).
Second-degree AV block is characterized by atrial impulses (generally occurring at a regular rate) that fail to conduct to the ventricles in 1 of the following 4 ways.
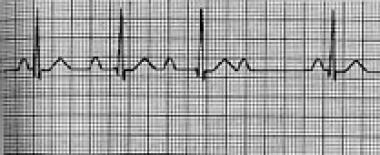
The first form of second-degree AV block is Mobitz I second-degree AV block (Wenckebach block), which consists of progressive prolongation of the PR interval with the subsequent occurrence of a single nonconducted P wave that results in a pause. The pause is shorter than the sum of any 2 consecutive conducted beats (R-R interval).
An episode of Mobitz I AV block usually consists of 3-5 beats, with a ratio of nonconducted to conducted beats of 4:3, 3:2, and so forth (see the image below). The block is generally in the AV node but can occasionally occur in the His-Purkinje system and is termed intrahisian or infrahisian Wenckebach (depending if the block occurs within or below the His-Purkinje system).
The second form is Mobitz II second-degree AV block, which is characterized by a constant PR interval followed by sudden failure of a P wave to be conducted to the ventricles, so that either an occasional dropped P wave or a regular conduction pattern of 2:1 (2 conducted and 1 blocked), 3:1 (3 conducted and 1 blocked), and so on is observed (see the image below).

The third form is high-grade AV block, which consists of multiple P waves in a row that should conduct, but do not. The conduction ratio can be 3:1 or higher, and the PR interval of conducted beats is constant. This is a distinct form of complete AV block, in that the P waves that conduct to the QRS complexes occur at fixed intervals. For complete AV block, no relationship exists between the P waves and QRS complexes.
The fourth form is 2:1 AV block. This could be either Mobitz I or Mobitz II, but distinguishing one variety from the other is nearly impossible.
Third-degree AV block is diagnosed when no supraventricular impulses are conducted to the ventricles. P waves on the rhythm strip reflect a sinus node rhythm independent from QRS wave complexes. The QRS complexes represent an escape rhythm, either junctional or ventricular. The escape rhythm originating from the junctional or high septal region is characterized by narrow QRS complexes at a rate of 40-50 beats/min, whereas escape rhythm from low ventricular sites is characterized by broad QRS complexes at a rate of 30-40 beats/min.
No relationship exists between the rhythm of P waves and the rhythm of QRS complexes in third-degree AV block. The frequency of P waves (atrial rate) is higher than the frequency of QRS complexes (ventricular rate) (see the image below).

AV dissociation is a rhythm identified by atrial and ventricular activation occurring from different pacemakers. AV dissociation does not indicate the presence of AV block and is distinctly different. Ventricular activation may be from either junctional pacemakers or infranodal.
AV dissociation can occur in the presence of intact AV conduction, especially when rates of the pacemaker, either junctional or ventricular, exceed the atrial rate. Third-degree AV block can occur with AV dissociation. However, in AV dissociation without AV block, the ventricular rate can exceed the atrial rate and conduction can occasionally occur dependent on the timing between the P wave and the QRS complex.
AV block may also occur in patients with atrial fibrillation (see the Atrial Fibrillation Center). Regular R-R intervals are possible in the presence of AV block (generally at slow regular rates).
Pathophysiology
The atrioventricular node (AVN) is part of the conduction system of the heart that allows electrical impulses to be transmitted from the sinus node via atrial tissue (intra-atrial fascicles) to the ventricles. This node consists of 3 parts—atrionodal (transitional zone), nodal (compact portion), and nodal-His (penetrating His bundle). The nodal portion causes the slowest conduction.
The AVN is supplied by the right coronary artery (90%) or by the circumflex artery (10%) and is innervated by both sympathetic and parasympathetic fibers. It receives impulses anteriorly via the intra-atrial fibers in the septum and posteriorly via the crista terminalis. Impulses arriving at the AVN are transmitted to the ventricle in a 1:1 ratio. As faster impulses arrive, the conduction to the ventricles slows; this is called decremental conduction.
The His-Purkinje system is composed of 2 bundles of Purkinje fibers (the left and right bundle) that conduct electrical impulses to allow rapid ventricular activation. The His-Purkinje system is yet another location where AV block may occur.
First-degree AV block and second-degree Mobitz I AV block usually involve a delay at the level of the AVN, whereas second-degree Mobitz II AV block generally involves blockage in the His bundle or lower regions of the conduction system. Third-degree AV block involves conduction disturbances in the AV node or the His-Purkinje system.
In most cases of complete AV block, an escape rhythm originates from the ventricles, with wide QRS complexes at a low regular rate of 30-40 beats/min. A higher anatomic location of the block results in a higher location of the escape rhythm pacemaker, a faster escape rhythm (40-60 beats/min in the region of His bundle), and a narrower QRS duration.
Etiology
Delay or lack of conduction through the AV node has multiple causes.
First-degree AV block and Mobitz I (Wenckebach) second-degree AV block may occur in healthy, well-conditioned people as a physiologic manifestation of high vagal tone. Mobitz I AV block also may occur physiologically at high heart rates (especially with pacing) as a result of increased refractoriness of the AVN, which protects against conducting an accelerated arrhythmia to the ventricles.
AV block may be caused by acute myocardial ischemia or infarction. Inferior myocardial infarction may lead to third-degree block, usually at the AVN level; this may occur through other mechanisms via the Bezold-Jarisch reflex. Anterior myocardial infarction usually is associated with third-degree block resulting from ischemia or infarction of bundle branches.
Degenerative changes in the AVN or bundle branches (eg, fibrosis, calcification, or infiltration) are the most common cause of nonischemic AV block. Lenegre-Lev syndrome is an acquired complete heart block due to idiopathic fibrosis and calcification of the electrical conduction system of the heart. It is most commonly seen in the elderly and is often described as senile degeneration of the conduction system and may lead to third-degree AV block.
In 1999, degenerative changes in the AV conduction system were linked to mutations of the SCN5A sodium channel gene (mutations of the same gene may lead to congenital long QT syndrome type 3 and to Brugada syndrome).
Infiltrative myocardial diseases resulting in AV block include sarcoidosis, myxedema, hemochromatosis, and progressive calcification related to mitral or aortic valve annular calcification. Endocarditis and other infections of the myocardium, such as Lyme disease with active infiltration of the AV conduction system, may lead to varying degrees of AV block. Systemic diseases, such as ankylosing spondylitis and Reiter syndrome, may affect the AV nodal conducting tissue.
Surgical procedures (eg, aortic valve replacement and congenital defect repair) may cause AV block, as may other therapeutic procedures (eg, AV node ablation and alcohol septal ablation in patients with obstructive hypertrophic cardiomyopathy). Patients with corrected transposition of the great vessels have anterior displacement of the AVN and are prone to develop complete heart block during right heart catheterization or surgical manipulation.
A variety of drugs may affect AV conduction. The most common of these include digitalis glycosides, beta-blockers, calcium channel blockers, adenosine, and other antiarrhythmic agents.
Source emedicine.com
Duc Tin Surgical CLinic
Tin tức liên quan

Performance diagnostique de l’interféron gamma dans l’identification de l’origine tuberculeuse des pleurésies exsudatives

A Mixed Phenotype of Airway Wall Thickening and Emphysema Is Associated with Dyspnea and Hospitalization for Chronic Obstructive Pulmonary Disease.

Radiological Approach to Asthma and COPD-The Role of Computed Tomography.

Significant annual cost savings found with UrgoStart in UK and Germany

Thrombolex announces 510(k) clearance of Bashir catheter systems for thromboembolic disorders
Phone: (028) 3981 2678
Mobile: 0903 839 878 - 0909 384 389







