Background
Venous air embolism (VAE), a subset of gas embolism, is an entity with the potential for severe morbidity and mortality. Venous air embolism is a predominantly iatrogenic complication that occurs when atmospheric gas is introduced into the systemic venous system. In the past, this medical condition was mostly associated with neurosurgical procedures conducted in the sitting position.
Venous air embolism (VAE), a subset of gas embolism, is an entity with the potential for severe morbidity and mortality. Venous air embolism is a predominantly iatrogenic complication that occurs when atmospheric gas is introduced into the systemic venous system. In the past, this medical condition was mostly associated with neurosurgical procedures conducted in the sitting position.
More recently, venous air embolism has been associated with central venous catheterization, penetrating and blunt chest trauma, high-pressure mechanical ventilation, thoracocentesis, hemodialysis, and several other invasive vascular procedures.
Venous air embolism (VAE) has also been observed during diagnostic studies, such as during radiocontrast injection for computerized tomography. The use of gases such as carbon dioxide and nitrous oxide during medical procedures and exposure to nitrogen during diving accidents can also result in VAE. In addition, apparent cases of VAE resulting from pressurized, intravenous infusion of normal saline have been reported in professional football players. Many cases of VAE are subclinical with no adverse outcome and thus go unreported. Usually, when symptoms are present, they are nonspecific, and a high index of clinical suspicion of possible VAE is required to prompt investigations and initiate appropriate therapy.
Pathophysiology
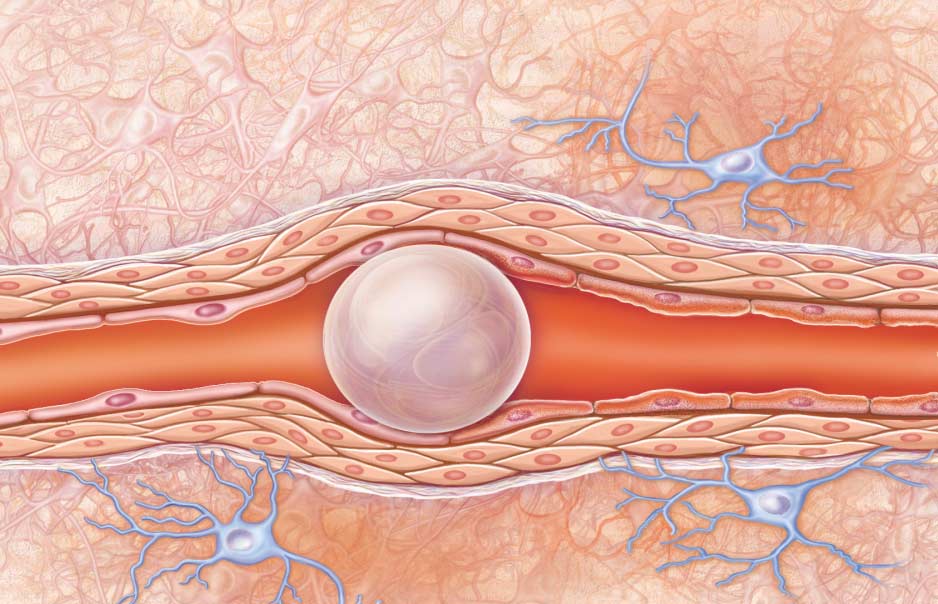
Two preconditions must exist for venous air embolism to occur: (1) a direct communication between a source of air and the vasculature and (2) a pressure gradient favoring the passage of air into the circulation.
The key factors determining the degree of morbidity and mortality in venous air emboli are related to the volume of gas entrainment, the rate of accumulation, and the patient’s position at the time of the event.
Generally, small amounts of air are broken up in the capillary bed and absorbed from the circulation without producing symptoms. Traditionally, it has been estimated that more than 5 mL/kg of air displaced into the intravenous space is required for significant injury (shock or cardiac arrest) to occur. However, complications have been reported with as little as 20 mL of air (the length of an unprimed IV infusion tubing) that was injected intravenously. The injection of 2 or 3 mL of air into the cerebral circulation can be fatal. Furthermore, as little as 0.5 mL of air in the left anterior descending coronary artery has been shown to cause ventricular fibrillation. Basically, the closer the vein of entrainment is to the right heart, the smaller the lethal volume is.
Rapid entry or large volumes of air entering the systemic venous circulation puts a substantial strain on the right ventricle, especially if this results in a significant rise in pulmonary artery (PA) pressures. This increase in PA pressure can lead to right ventricular outflow obstruction and further compromise pulmonary venous return to the left heart. The diminished pulmonary venous return will lead to decreased left ventricular preload with resultant decreased cardiac output and eventual systemic cardiovascular collapse.
With venous air embolism (VAE), resultant tachyarrhythmias are frequent, but bradyarrhythmias can also occur.
The rapid ingress of large volumes of air (>0.30 mL/kg/min) into the venous circulatory system can overwhelm the air-filtering capacity of the pulmonary vessels, resulting in a myriad of cellular changes. [3] The air embolism effects on the pulmonary vasculature can lead to serious inflammatory changes in the pulmonary vessels; these include direct endothelial damage and accumulation of platelets, fibrin, neutrophils, and lipid droplets.
Secondary injury as a result of the activation of complement and the release of mediators and free radicals can lead to capillary leakage and eventual noncardiogenic pulmonary edema.
Alteration in the resistance of the lung vessels and ventilation-perfusion mismatching can lead to intra-pulmonary right-to-left shunting and increased alveolar dead space with subsequent arterial hypoxia and hypercapnia.
Arterial embolism as a complication of venous air embolism (VAE) can occur through direct passage of air into the arterial system via anomalous structures such as an atrial or ventricular septal defect, a patent foramen ovale, or pulmonary arterial-venous malformations. This can cause paradoxical embolization into the arterial tree. The risk for a paradoxical embolus seems to be increased during procedures performed in the sitting position.
Air embolism has also been described as a potential cause of the systemic inflammatory response syndrome (case report), triggered by the release of endothelium derived cytokines.
Etiology
In order for venous air embolism (VAE) to occur, the following two physical preconditions for the entry of gas into the venous system must be met:
-
A direct communication between a source of air/gas and the vasculature (incising of noncollapsed veins) must exist.
-
A pressure gradient (subatmospheric pressure in the vessels) favoring the passage of air into the circulation must be present.
Classically, venous air embolism has been recognized as occurring in the context of decompression illness in divers, aviators, and astronauts. Barotrauma and air emboli complicate an estimated 7 of every 100,000 dives. [15, 16] However, the most common cause of VAE is iatrogenic.
Surgical procedures
Surgical procedures are the primary cause of VAE. Neurosurgical procedures, especially those performed in the Fowler’s (sitting) position, and otolaryngological interventions are the two most common surgeries complicated by VAE. Note the following:
-
The incidence of mild or clinically silent VAE during neurosurgical procedures has been estimated to range between 10% in cervical laminectomy surgeries where the patients are in the prone position, and 80% during posterior fossa surgeries (eg, repair of cranial synostosis) where patients are placed in the Fowler’s position.
-
VAE poses a risk anytime the surgical wound is elevated more than 5 cm above the right atrium. The presence of numerous, large, noncompressed, venous channels in the surgical field (especially during cervical procedures and craniotomies that breach the dural sinuses) also increase the risk of VAE.
-
Entrainment of air/gas facilitated by the patient's intraoperative position causing VAE, may result from other surgical procedures. These include, craniofacial surgery, dental implant surgery, vascular procedures (eg, endarterectomies), liver transplantation, orthopedic procedures (eg, hip replacement, spine surgery, arthroscopy), lateral decubitus thoracotomy, genitourinary surgeries in the Trendelenburg position, and surgeries involving tumors/malformations with high degree of vascularity or compromised vessels, as in the context of trauma.
-
A preliminary study by Longatti et al suggests that carbon dioxide field flooding (ie, carbox dioxide–enriched surgical microenvironment) reduces the hemodynamic effects of VAE occurring in the sitting position, which the investigators attribute to the better solubility and improved tolerance of the arterial carbon dioxide emboli compared to air emboli.
Obstetric/gynecologic procedures, laparoscopy
Obstetric/gynecologic procedures (cesarean delivery) and laparoscopic surgeries each carry their own risk for VAE. Although this risk is commonly not considered, they each have a reported associated incidence risk of VAE greater than 50%. The risk of VAE during cesarean deliveries may be highest when the uterus is exteriorized. The risk of VAE in laparoscopic surgery may require an inadvertent opening of vascular channels through surgical manipulation rather than simply resulting from a complication of insufflation. Both of these surgical procedures have been associated with intraoperative mortality as a direct sequelae of air emboli. Despite this, the potential for venous air embolism is often ignored in laparoscopic surgery and cesarean delivery.
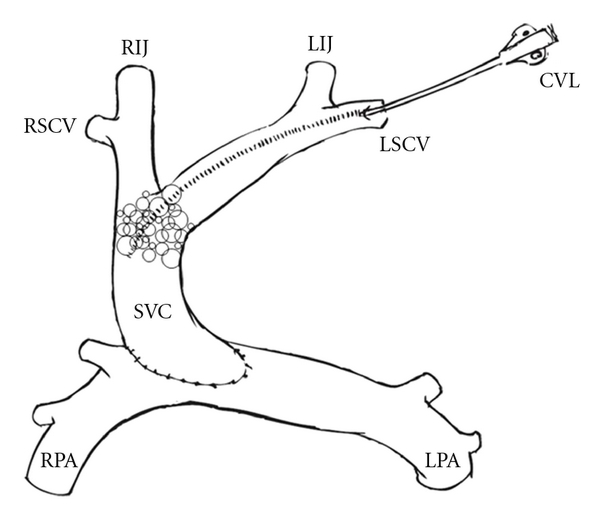
Iatrogenic creation of a pressure gradient
Venous air embolism may also result from the iatrogenic creation of a pressure gradient for air entry. Procedures causing such a pressure gradient include lumbar puncture (case report), peripheral intravenous lines, and central venous catheters.
Source emedicine.com
Duc Tin Sugical Clinic
Tin tức liên quan

Performance diagnostique de l’interféron gamma dans l’identification de l’origine tuberculeuse des pleurésies exsudatives

A Mixed Phenotype of Airway Wall Thickening and Emphysema Is Associated with Dyspnea and Hospitalization for Chronic Obstructive Pulmonary Disease.

Radiological Approach to Asthma and COPD-The Role of Computed Tomography.

Significant annual cost savings found with UrgoStart in UK and Germany

Thrombolex announces 510(k) clearance of Bashir catheter systems for thromboembolic disorders
Phone: (028) 3981 2678
Mobile: 0903 839 878 - 0909 384 389







