Overview
Venous insufficiency resulting from superficial reflux because of varicose veins is a serious problem that usually progresses inexorably if left untreated. When the refluxing circuit involves failure of the primary valves at the saphenofemoral junction, treatment options for the patient are limited, and early recurrences are the rule rather than the exception.
Venous insufficiency resulting from superficial reflux because of varicose veins is a serious problem that usually progresses inexorably if left untreated. When the refluxing circuit involves failure of the primary valves at the saphenofemoral junction, treatment options for the patient are limited, and early recurrences are the rule rather than the exception.
In the historical surgical approach, ligation and division of the saphenous trunk and all proximal tributaries are followed either by stripping of the vein or by avulsion phlebectomy. Proximal ligation requires a substantial incision at the groin crease. Stripping of the vein requires additional incisions at the knee or below and is associated with a high incidence of minor surgical complications. Avulsion phlebectomy requires multiple 2- to 3-mm incisions along the course of the vein and can cause damage to adjacent nerves and lymphatic vessels.
Endovenous ablation has replaced stripping and ligation as the technique for elimination of saphenous vein reflux. One of the endovenous techniques is a radiofrequency-based procedure. Newer methods of delivery of radiofrequency were introduced in 2007. Endovenous procedures are far less invasive than surgery and have lower complication rates. The procedure is well tolerated by patients, and it produces good cosmetic results. Excellent clinical results are seen at 4-5 years, and the long-term efficacy of the procedure is now known with 10 years of experience. The original radiofrequency endovenous procedure was cleared by the US Food and Drug Administration (FDA) in March 1999.
Endovenous techniques (endovenous laser therapy, radiofrequency ablation, and endovenous foam sclerotherapy) clearly are less invasive and are associated with fewer complications compared with more invasive surgical procedures, with comparable or greater efficacy.
Technology
The original radiofrequency endovenous ablation system worked by thermal destruction of venous tissues using electrical energy passing through tissue in the form of high-frequency alternating current. This current was converted into heat, which causes irreversible localized tissue damage. Radiofrequency energy is delivered through a special catheter with deployable electrodes at the tip; the electrodes touch the vein walls and deliver energy directly into the tissues without coagulating blood. The newest system, called ClosureFast, delivers infrared energy to vein walls by directly heating a catheter tip with radiofrequency energy.
Energy delivery
In the original radiofrequency catheter system, the catheter was pulled through the vein while feedback is controlled with a thermocouple to a temperature of 85°C to avoid thermal injury to the surrounding tissues or carbonization of the vein wall. With the new system, the catheter is held in place while energy heats the catheter to a specified temperature of 120ºC. As the vein is denatured by heat, it contracts around the catheter.
With the previous-generation radiofrequency system, as shrinkage and compaction of tissue occurred, impedance was decreased which decreased heat generation; however, this is no longer the case. Only the temperature of the catheter metal core is monitored as it delivers heat to the vessel wall in 20-second increments. Previously, the radiofrequency generator could be programmed to rapidly shutdown when impedance rose, thus assuring minimal heating of blood but efficient heating of the vein wall. In the present system, catheter core temperature is monitored and adjusts energy to keep the core at 120 º C. Heat delivered to the vein wall causes the vessel to shrink in the treated area, and the catheter is gradually withdrawn along the course of the vein until the entire vessel has been treated. This is performed in 7-cm segments.
The image below demonstrates a schematic diagram of the process.
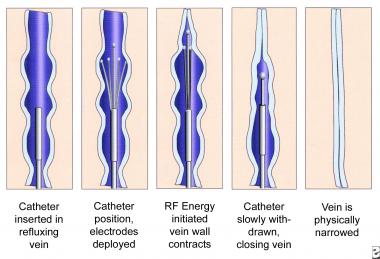
Schematic images of the process of radiofrequency endovenous occlusion.

Radiofrequency ablation console (VNUS Medical Technologies) showing (left to right) time, temperature, impedance, and power (in watts).
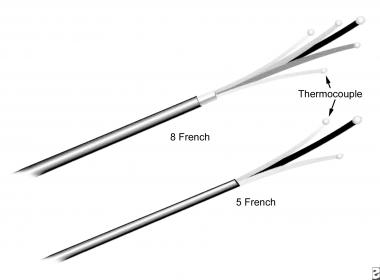
Closure radiofrequency ablation catheters in 2 sizes (VNUS Medical Technologies).
Catheters
Many different radiofrequency ablation catheters are available for medical applications, but the Closure catheter, manufactured by VNUS Medical Technologies, is the only commercially available radiofrequency ablation system designed for venous ablation. The image below shows the Closure console, and the second image below shows 2 sizes of radiofrequency ablation catheters.
Radiofrequency ablation console (VNUS Medical Technologies) showing (left to right) time, temperature, impedance, and power (in watts).
Closure radiofrequency ablation catheters in 2 sizes (VNUS Medical Technologies).
Histologic Findings
Immediately after treatment, biopsy specimens show a significant reduction in the size of the vein lumen, with denudation of endothelium, thrombus formation, thickened vessel walls, loss of collagen birefringence, and inflammatory changes. The zone of thermal damage is limited to 2 mm beyond the point of contact with the electrodes.
In more than 90% of patients, biopsy specimens demonstrate complete occlusion of the vein lumen 6 weeks after treatment. The lumen is completely ablated in most areas, with some portions of the vessel demonstrating a small residual lumen containing organized fibrous thrombi. Birefringence is present, and new collagen growth is evident.
Technique
Radiofrequency ablation catheters cannot be easily passed along a tortuous superficial vein; therefore, the procedure is principally of use in the treatment of truncal varicose veins, such as the great saphenous vein. Radiofrequency ablation is also used with small saphenous vein incompetence.
Preprocedure
Duplex ultrasonography is used to confirm and map all areas of reflux and to trace the path of the refluxing great saphenous trunk from the saphenofemoral junction down the leg to the lower thigh or upper part of the calf. The vein, the saphenofemoral junction, and the anticipated entry point are marked in some way on the skin. An appropriate entry point is selected just above or just below the knee, at a point permitting cannulation of the vessel with a 16-gauge needle introducer.
Procedure
The leg is prepared and draped, and a superficial local anesthetic agent is used to anesthetize the site of cannulation. Needle puncture of the vessel is guided by duplex ultrasonography. The Seldinger technique is used to place a guidewire into the vessel, and an introducer sheath is passed over the guidewire, which is removed. The ClosureFast catheter is passed through the sheath, and the tip is advanced to 2 cm below the saphenofemoral junction under duplex ultrasonographic visualization.
With ultrasonographic guidance, a local anesthetic agent is injected into the tissues surrounding the great saphenous vein above and within its fascial sheath. The anesthetic is injected along the entire course of the vein from the catheter insertion point to the saphenofemoral junction. In most patients, 200-400 mL of lidocaine 0.1% is sufficient to both anesthetize and compress the vessel. Note the importance of delivering the anesthetic agent in the correct intrafascial location, with a volume sufficient to compress the vein and dissect it away from other structures, such as nerves, along its entire length.
Duplex ultrasonography is used to position the catheter tip 2 cm below the level of the terminal valve of the saphenofemoral junction. The catheter must not extend into the femoral vein because injury to the femoral vein may cause deep vein thrombosis.
In the previous radiofrequency ablation system, when the console is switched on and the test mode is activated, the baseline impedance should be 250-300 ohms and the baseline temperature should be 32-37°C. When radiofrequency energy is applied, the thermocouple temperature should rise to 80-85°C within 10-15 seconds. In the new system, when the radiofrequency is activated, the catheter core temperature should rapidly rise to 120ºC and should be sustained for 15 seconds of the 20-second pulse cycle. If the temperature does not rise quickly, a malpositioned catheter tip should be strongly suspected.
In the previous system, after the temperature reaches 85°C and remains constant for 15 seconds, the catheter tip is slowly withdrawn at a rate of approximately 1 cm per minute (1 mm every 6 seconds). In the new system, two 20-second cycles are performed in the proximal section, after which the catheter is withdrawn 7 cm as per catheter markings. The next 20-second cycle is repeated once, and, if 120ºC is maintained, the catheter is then withdrawn another 7 cm until the entire vein is treated.
When proper tumescent anesthesia is applied, the patient should never experience a sudden heat sensation. If this happens, more anesthesia is injected.
Postprocedure
Posttreatment duplex ultrasonography confirms the contraction of the vessel and the absence of flow along the entire length of the treated vessel. In the previous system, if persistent flow is observed, the procedure may be repeated immediately, provided the catheter can still be easily passed along the vessel to the desired site of treatment. In the new system of ClosureFast, the procedure is not repeated because the targeted vessel typically shows no flow.
Source emedicine
Duc Tin Surgical Clinic
Tin tức liên quan

Performance diagnostique de l’interféron gamma dans l’identification de l’origine tuberculeuse des pleurésies exsudatives

A Mixed Phenotype of Airway Wall Thickening and Emphysema Is Associated with Dyspnea and Hospitalization for Chronic Obstructive Pulmonary Disease.

Radiological Approach to Asthma and COPD-The Role of Computed Tomography.

Significant annual cost savings found with UrgoStart in UK and Germany

Thrombolex announces 510(k) clearance of Bashir catheter systems for thromboembolic disorders
Phone: (028) 3981 2678
Mobile: 0903 839 878 - 0909 384 389







