Follow-up Care
Compression is of vital importance after any venous procedure. Compression is effective in reducing postoperative bruising and tenderness, and it can also reduce the risk of venous thromboembolism in both the treated leg and the untreated leg.
A class II (30- to 40-mm Hg gradient) compression stocking is applied to the treated leg, and, if the patient is willing, it is also applied to the untreated leg. Bed rest and lifting of heavy objects are forbidden, and normal activity is encouraged.
The patient is reevaluated 3-7 days after the operation, at which time duplex ultrasonography should demonstrate a closed greater saphenous vein and no evidence of thrombus in the femoral, popliteal, or deep veins of the calf.
At 6 weeks, an examination should reveal clinical resolution of truncal varices, and an ultrasonographic evaluation should demonstrate a completely closed vessel and no remaining reflux. If any residual open segments are noted, sclerotherapy is performed under ultrasonographic guidance.
Complications
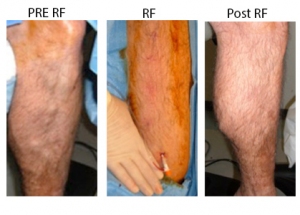
Reported complications of the procedure are rare. Local paresthesias can occur from perivenous nerve injury but are usually temporary. Thermal injury to the skin was reported in clinical trials when the volume of local anesthetic was not sufficient to provide a buffer between the skin and a particularly superficial vessel, especially below the knee. Progression of thrombus from local superficial phlebitis has occasionally been observed when compression was not used. The greatest current area of concern is deep vein thrombosis, with one 2004 study documenting deep vein thrombus requiring anticoagulation in 16% of 73 limbs treated with a radiofrequency ablation procedure.
Outcomes
Published results show a high early success rate with a very low subsequent recurrence rate up to 10 years after treatment. Early and mid range results are comparable to those obtained with other endovenous ablation techniques. The authors’ overall experience has been a 90% success rate, with rare patients requiring a repeat procedure in 6-12 months. Overall efficacy and lower morbidity have resulted in endovenous ablation techniques replacing surgical stripping.
Patient satisfaction is high and downtime is minimal, with 95% of patients reporting they would recommend the procedure to a friend.
A study by Proebstle et al found that at 5-year follow-up, radiofrequency segmental thermal ablation remained a successful treatment for over 90% of patients who underwent the therapy for incompetent great saphenous veins. The vein occlusion rate was 91.9% at last follow-up, with the Venous Clinical Severity Score changing from 3.9 at baseline to 0.6 at 1 year, 0.9 at 3 years, and 1.3 at 5 years.
A study by Bush et al indicated that perforating veins are the most frequent cause of recurrent varicose veins after radiofrequency or laser ablation. Of 2380 patients involved in the study, 164 had a recurrence of varicose veins, with the median period to recurrence being 3 years. Among the patients who experienced recurrence, 159 had undergone great saphenous vein ablation as their initial treatment, including 52 who had concurrently undergone small saphenous vein or anterior accessory great saphenous vein ablation. Along with perforating veins (64% of patients), the most common factors behind varicose vein recurrence were as follows :
-
Recanalized great saphenous vein (29% of patients)
-
New anterior accessory great saphenous vein reflux (24% of patients)
-
New small saphenous vein reflux (15% of patients)
It was also found that a higher rate of recanalization occurred with radiofrequency ablation than with the laser procedure.
A study by Bozoglan et al also suggested that endovenous laser ablation may have some advantages over radiofrequency ablation of varicose veins. The study included 60 patients with bilateral saphenous vein insufficiency, each of whom had one leg treated with the radiofrequency procedure and the other treated with laser therapy. The investigators found that the recanalization rate was 6.8% in the legs treated with radiofrequency ablation, compared with 0% in the laser-treated legs. Moreover, 51.7% of patients were satisfied with endovenous laser ablation, versus 31.0% who were satisfied with radiofrequency ablation (and 17.2% who were satisfied with both procedures).
Source emedicine.com
Duc Tin Surgical Clinic
Tin tức liên quan

Performance diagnostique de l’interféron gamma dans l’identification de l’origine tuberculeuse des pleurésies exsudatives

A Mixed Phenotype of Airway Wall Thickening and Emphysema Is Associated with Dyspnea and Hospitalization for Chronic Obstructive Pulmonary Disease.

Radiological Approach to Asthma and COPD-The Role of Computed Tomography.

Significant annual cost savings found with UrgoStart in UK and Germany

Thrombolex announces 510(k) clearance of Bashir catheter systems for thromboembolic disorders
Phone: (028) 3981 2678
Mobile: 0903 839 878 - 0909 384 389







