Heart Failure (HF) is defined, clinically, as a syndrome in which patients have typical symptoms (e.g. breathlessness, ankle swelling, and fatigue) and signs (e.g. elevated jugular venous pressure, pulmonary crackles, and displaced apex beat) resulting from an abnormality of cardiac structure or function.
Heart Failure (HF) is defined, clinically, as a syndrome in which patients have typical symptoms (e.g. breathlessness, ankle swelling, and fatigue) and signs (e.g. elevated jugular venous pressure, pulmonary crackles, and displaced apex beat) resulting from an abnormality of cardiac structure or function.
Demonstration of an underlying cardiac cause is central to the diagnosis of HF. This is usually myocardial disease causing systolic ventricular dysfunction. However, abnormalities of ventricular diastolic function or of the valves, pericardium, endocardium, heart rhythm, and conduction can also cause HF (and more than one abnormality can be present).
Mathematically, Lelf Ventricular Ejection Fraction (EF) is the stroke volume (which is the end diastolic volume minus the end systolic volume) divided by the end diastolic volume. For example, in patients with systolic dysfunction in reduced contraction and emptying of the left ventricle, stroke volume is maintained by an increase in end diastolic volume. The heart ejects a smaller fraction of a larger volume. The more severe the systolic dysfunction, the more the EF is reduced from normal and the greater the end diastolic and end systolic volumes.
The EF is considered important in HF, not only because of its prognostic importance (the lower the EF, the poorer the survival) but also because most clinical trials selected patients based upon EF (usually measured using a radionuclide technique or echocardiography). The major trials in patients with HF and a reduced EF (HF-REF), or ‘systolic HF’, mainly enrolled patients with an EF ≤ 35%, and it is only in these patients that effective therapies have been demonstrated to date.
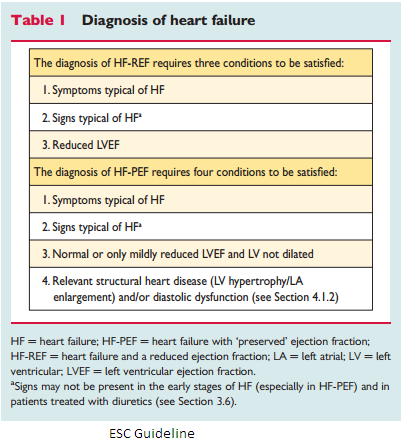
The term HF with ‘preserved’ EF (HF-PEF) was created to describe patients who did not have an entirely normal EF (generally considered to be >50%) but also did not have a major reduction in systolic function either. The diagnosis of HF-PEF is more difficult than the diagnosis of HF-REF because it is largely one of exclusion diagnosis. In the other hand, potential non-cardiac disease causes of the patient’s symptoms (such as anaemia or chronic lung disease) must first be discounted. These patients usually do not have a dilated heart and many patients have an increase in LV wall thickness and increased left atrial (LA) size. Most patients have evidence of diastolic dysfunction which is generally accepted as the likely cause of HF.
It is important to note that EF values and normal ranges are dependent on the imaging technique employed, method of analysis, and operator. Other, more sensitive measures of systolic function may show abnormalities in patients with a preserved or even normal EF, hence, the preference for stating preserved or reduced EF over preserved or reduced ‘systolic function’.
ESC Guideline
Duc Tin clinic
Tin tức liên quan

Performance diagnostique de l’interféron gamma dans l’identification de l’origine tuberculeuse des pleurésies exsudatives

A Mixed Phenotype of Airway Wall Thickening and Emphysema Is Associated with Dyspnea and Hospitalization for Chronic Obstructive Pulmonary Disease.

Radiological Approach to Asthma and COPD-The Role of Computed Tomography.

Significant annual cost savings found with UrgoStart in UK and Germany

Thrombolex announces 510(k) clearance of Bashir catheter systems for thromboembolic disorders
Phone: (028) 3981 2678
Mobile: 0903 839 878 - 0909 384 389







