I.Technique
ELA procedure for through the sheath laser fiber kits
- Perform preprocedural DUS for mapping of the venous segments to be treated. Mark the course of the vein(s) to be treated and important anatomical landmarks associated with the ablation on the skin, including the proposed venous access site(s) and deep vein junctions. The access site is ideally at the inferior end of the incompetent segment or segments of the treated vein. In most cases, the entire incompetent segment(s) can be treated with 1 puncture. If microphlebectomy will be performed along with ELA, the veins to be removed should be marked at this time as well.
- Prepare the operative tray and equipment. Aside from the thermal ablation device and a venous access kit, only basic supplies such as gauze, a sterilizing solution, sterile barriers, and the tumescent solution, with delivery syringes and needle and an ultrasound probe cover, are needed.
- Carry out sterile preparation and draping of the leg to be treated. Preprocedural antibiotics are not necessary in almost all circumstances as the procedure is performed sterilely and is considered clean.
- Visualize the access site with DUS. Placing the patient in a reverse Trendelenburg or partly sitting position prior to the venous puncture keeps the vein more distended and may facilitate venous access.
- Anesthetize the access site. Nick the skin just large enough to facilitate entry of the sheath through the skin.
- Insert the access needle into the great saphenous vein (GSV) under sonographic guidance. Use of a 21G puncture set, as discussed previously, is preferred particularly when the target vein is < 4 mm in diameter when supine. Cutdown is rarely needed and usually only if percutaneous access fails.
- Place a 0.035-in guidewire into the vein.
- Confirm intravenous placement with ultrasonography.
- Place the introducer sheath over the wire.
- Position the sheath for ELA to the starting point for ablation. Some physicians typically advance the ELA sheath beyond the starting point and later withdraw it with the laser fiber to the starting spot. The movement of withdrawal helps in to accurately identify the tip and position it at the starting point.
- Remove the wire and its dilator if one is used with the sheath. Check for venous return by aspirating the syringe attached to the sheath and flush. Recognize that the sheath tip may be against the vein wall and may not aspirate freely. Also realize that when flushing, microbubbles of air introduced into the vein may produce an acoustic shadow that may limit the ability to see venous detail and device positions.
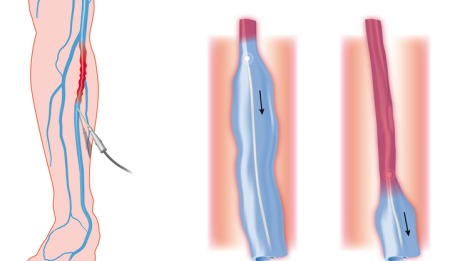
- Introduce the laser fiber into the sheath so that the fiber reaches the sheath tip. There is generally a mark on the fiber to show this. Then fix the laser fiber and carefully pull back the sheath to expose about 2–3 cm of fiber. Then withdraw the entire sheath-laser fiber to the ablation starting spot.
- Fine tune the location of the tip of the laser fiber to just below the superficial epigastric vein, anterior accessory GSV (AAGSV), or other large normal junctional vein for the GSV, and just below the thigh extension junction with the short saphenous vein (SSV) for SSV ablations. Some operators choose to position the laser fiber 1-3 cm below the saphenofemoral junction (SFJ) without consideration of the position of the junctional branches. No data support superiority of any of the above procedures in terms of ablation success, junctional recurrences, or common femoral vein thrombosis post procedure. See the image below.
- Longitudinal (sagittal) duplex ultrasound image of the saphenofemoral junction during the positioning of the tip of a laser fiber during an endovenous laser ablation. The laser tip is in the greater saphenous vein (GSV) just beyond the superficial epigastric vein (SEV) origin and is marked by the arrow. FV=femoral vein.
- Connect the laser fiber to its generator and confirm that the tip is in the correct general location by viewing the visible light aiming beam that can be delivered into the laser fiber tip and visualized through the skin. This is an additional way to ensure that the tip of the laser is being visualized accurately and that the laser connections were made appropriately. If the light is not seen in the expected location, troubleshoot the position of the laser or the connection to the laser to understand why.
- Administer tumescent anesthesia with ultrasound guidance after the patient has been placed into the Trendelenburg position to help drain the vein.
- Place appropriate laser safety goggles on everyone in the procedure room and use other appropriate laser safety measures. Connect the laser fiber to the laser and verify proper laser settings. Setting recommendations vary, but aim to deliver at least 70–80 J/cm length of vein treated: at 14 W this is achieved with a pullback rate of 2 mm/s.
- Set the laser to continuous mode and select the power to be used. Re-verify placement of the laser tip with ultrasound.
- Activate the laser and withdraw the fiber and sheath at the speed that is dependent on the amount of energy you wish to deliver at the power setting selected with the laser in continuous mode. Many operators deliver 70-100 J/cm at 14 W in continuous mode at 810 nm throughout the length of the abnormal vein. For the GSV and AAGSV, the author uses more energy for the first 10-12 cm (140 J/cm) and less as the laser tip progresses lower down the leg (100 J/cm to the knee and 70 J/cm below the knee). This is done to ensure closure of the proximal vein segment just below the deep vein junction, where failure occurs most, and to decrease the risk of nerve injuries lower in the leg. For the SSV, the author uses about 112 J/cm for the first 3-4 cm, then 100 J/cm for the next 3-4 cm, and then 70 J/cm for the remaining vein.
- Stop laser energy delivery at the distal aspect of the vein and place the laser in standby mode.
- Remove the fiber/sheath from the vein. Be sure the entire fiber is removed to exclude the possibility of a fracture of the device intravascularly.
- Record the watts, laser on-time, total joules delivered, and length of the segment treated. Calculate the withdrawal rate and joules delivered per cm to ensure you have reached the targets for successful ablation.
II.Pearls
Technique considerations
The amount of thermal energy delivered is correlated to the success of ELA. With laser, energy deposition has been described as either that deposited per centimeter of vein length (J/cm) or as that deposited to the vein wall using a cylindrical approximation of the inner surface area of the vein (J/cm2), which can be considered a fluence equivalent. Durable vein occlusion was demonstrated in an observational series as more likely when the energy delivered exceeded 80 J/cm with a median observation of 30 weeks.High rates of vein occlusion and ultimate DUS disappearance was noted in a series where the thermal dose in each segment of the GSV was tailored to the diameter in that segment. The ranges of energies used to achieve durable ablation included 50 J/cm for veins ≤4.5 mm and 120 J/cm for veins >10 mm in diameter. No increase in complications was seen with any of the higher energy strategies.
To date, a prospective, randomized evaluation of the relationship of the different variables that can be controlled by the operator on the rate of anatomically successful vein obliteration and complication rates has not been performed. These variables include amount of laser energy deposition (J/cm or J/cm2), the rate of energy deposition (power setting), wavelength, and fiber design. Most combinations of treatments above the 70-80 J/cm seem to result in durable closure and some data support the notion that complications and adverse effects are not increased with energies up to 140 J/cm.
The differences between the current thermal ablation technologies are relatively small. Several retrospective analyses of observational data have demonstrated qualitatively similar occlusion and complication rates with a trend toward quicker treatments and better outcomes with ELA compared with the first generation RFA. In a study comparing Closure Fast (CF) and ELA, equivalent treatment times and anatomical success at 6 months were seen with slightly less immediate postprocedure bruising and postprocedure discomfort noted with CF.
ELA bruising and discomfort have been thought to be less with continuous mode laser deposition than with pulsed mode. Limited data suggest that these side effects may be lessened with the use of a laser fiber with its tip covered with a glass cap and metal sleeve as opposed to a bare fiber. This effectively makes the fiber larger and presumably more coagulating than cutting. The prevention of wall contact produced by the jacket-tipped fibers results in less postprocedure bruising and pain in one study that evaluated 20 patients who were treated with bare-tip fibers and jacket-tip fiber.
Excellent anatomic success of 90-100% occlusion rates has been shown for lasers with wavelengths between 810 and 1470 nm.Recently, the 1470-nm radial laser fiber has been shown to have the lowest amount of postprocedure bruising, pain, parasthesia, induration, and superficial phlebitis due to the water-specific wavelength that is thought to directly act on the vessel wall.Moreover, this study showed equivalent anatomic success of 99.6% closure at 1 year following use of the 1470-nm radial fiber.
Source emedicine.com
DUC TIN SURGICAL CLINIC
Tin tức liên quan

Performance diagnostique de l’interféron gamma dans l’identification de l’origine tuberculeuse des pleurésies exsudatives

A Mixed Phenotype of Airway Wall Thickening and Emphysema Is Associated with Dyspnea and Hospitalization for Chronic Obstructive Pulmonary Disease.

Radiological Approach to Asthma and COPD-The Role of Computed Tomography.

Significant annual cost savings found with UrgoStart in UK and Germany

Thrombolex announces 510(k) clearance of Bashir catheter systems for thromboembolic disorders
Phone: (028) 3981 2678
Mobile: 0903 839 878 - 0909 384 389







