1.Background
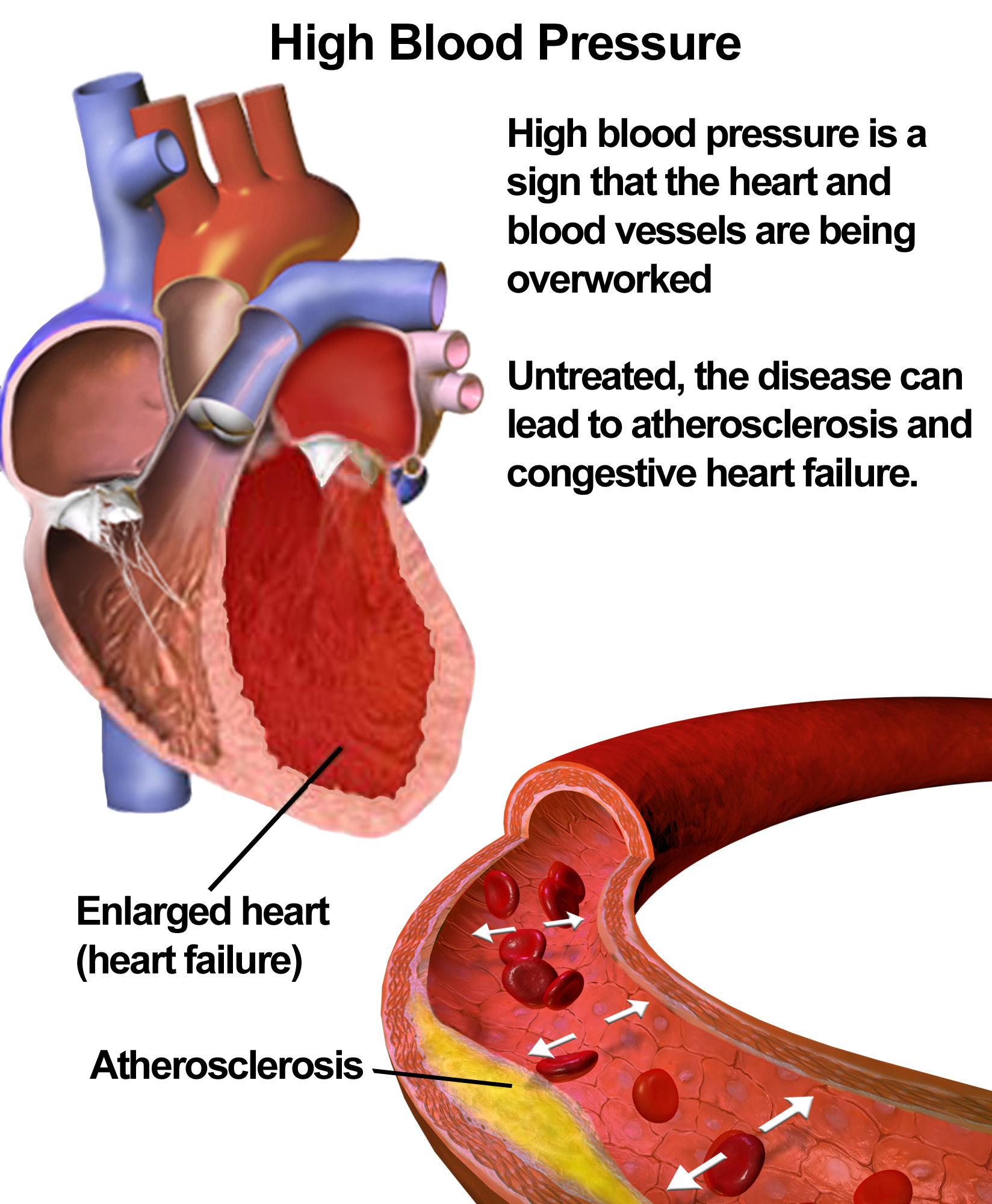
Hypertension is one of the most common worldwide diseases afflicting humans and is a major risk factor for stroke, myocardial infarction, vascular disease, and chronic kidney disease.
Despite extensive research over the past several decades, the etiology of most cases of adult hypertension is still unknown, and control of blood pressure is suboptimal in the general population. Due to the associated morbidity and mortality and cost to society, preventing and treating hypertension is an important public health challenge. Fortunately, recent advances and trials in hypertension research are leading to an increased understanding of the pathophysiology of hypertension and the promise for novel pharmacologic and interventional treatments for this widespread disease.
According to the American Heart Association (AHA), approximately 75 million adults in the United States are affected by hypertension, which is defined as a systolic blood pressure (SBP) of 140 mm Hg or more or a diastolic blood pressure (DBP) of 90 mm Hg or more or taking antihypertensive medication. Substantial improvements have been made with regard to enhancing awareness and treatment of hypertension. However, a National Health Examination Survey (NHANES) spanning 2005-2006 showed that 29% of US adults 18 years of age and older were hypertensive; 7% of hypertensive adults had never been told that they had hypertension.
Furthermore, of those with high blood pressure (BP), 78% were aware they were hypertensive, 68% were being treated with antihypertensive agents, and only 64% of treated individuals had controlled hypertension. In addition, data from NHANES 1999-2006 estimated that 30% of adults 20 years of age and older have prehypertension, defined as an untreated SBP of 120-139 mm Hg or untreated DBP of 80-89 mmHg.
Data from the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7), which was released in 2003, were relatively similar to the NHANES data. The JNC 7 noted that approximately 30% of adults were unaware of their hypertension; up to 40% of people with hypertension were not receiving treatment; and, of those treated, up to 67% did not have their BP controlled to less than 140/90 mm Hg
Hypertension is the most important modifiable risk factor for coronary heart disease (the leading cause of death in North America), stroke (the third leading cause), congestive heart failure, end-stage renal disease, and peripheral vascular disease. Therefore, health care professionals must not only identify and treat patients with hypertension but also promote a healthy lifestyle and preventive strategies to decrease the prevalence of hypertension in the general population.
2.Definition and classification
Defining abnormally high blood pressure (BP) is extremely difficult and arbitrary. Furthermore, the relationship between systemic arterial pressure and morbidity appears to be quantitative rather than qualitative. A level for high BP must be agreed upon in clinical practice for screening patients with hypertension and for instituting diagnostic evaluation and initiating therapy. Because the risk to an individual patient may correlate with the severity of hypertension, a classification system is essential for making decisions about aggressiveness of treatment or therapeutic interventions.
Based on recommendations of the JNC 7, the classification of BP (expressed in mm Hg) for adults aged 18 years or older is as follows :
- Normal: systolic lower than 120 mm Hg, diastolic lower than 80 mm Hg
- Prehypertension: systolic 120-139 mm Hg, diastolic 80-89 mm Hg
- Stage 1: systolic 140-159 mm Hg, diastolic 90-99 mm Hg
- Stage 2: systolic 160 mm Hg or greater, diastolic 100 mm Hg or greater
The classification above is based on the average of 2 or more readings taken at each of 2 or more visits after initial screening. Normal BP with respect to cardiovascular risk is less than 120/80 mm Hg. However, unusually low readings should be evaluated for clinical significance.
The Eighth Report of the JNC (JNC 8), released in December 2013, recommends less aggressive target blood pressures and treatment-initiation thresholds than the JNC7 for elderly patients and in patients younger than 60 years with diabetes and kidney disease, and no longer recommends just thiazide-type diuretics as initial therapy in most patients. In essence, the JNC 8 recommends treating to 150/90 mm Hg in patients over age 60 years; for everybody else, the goal BP is 140/90.
Prehypertension, a new category designated in the JNC 7 report, emphasizes that patients with prehypertension are at risk for progression to hypertension and that lifestyle modifications are important preventive strategies.
From another perspective, hypertension may be categorized as either essential or secondary. Primary (essential) hypertension is diagnosed in the absence of an identifiable secondary cause. Approximately 90-95% of adults with hypertension have primary hypertension, whereas secondary hypertension accounts for around 5-10% of the cases. However, secondary forms of hypertension, such as primary hyperaldosteronism, account for 20% of resistant hypertension (hypertension in which BP is >140/90 mm Hg despite the use of medications from 3 or more drug classes, 1 of which is a thiazide diuretic).
Especially severe cases of hypertension, or hypertensive crises, are defined as a BP of more than 180/120 mm Hg and may be further categorized as hypertensive emergencies or urgencies. Hypertensive emergencies are characterized by evidence of impending or progressive target organ dysfunction, whereas hypertensive urgencies are those situations without progressive target organ dysfunction
In hypertensive emergencies, the BP should be aggressively lowered within minutes to an hour by no more than 25%, and then lowered to 160/100-110 mm Hg within the next 2-6 hours. Acute end-organ damage in the setting of a hypertensive emergency may include the following :
- Neurologic: hypertensive encephalopathy, cerebral vascular accident/cerebral infarction, subarachnoid hemorrhage, intracranial hemorrhage
- Cardiovascular: myocardial ischemia/infarction, acute left ventricular dysfunction, acute pulmonary edema, aortic dissection, unstable angina pectoris
- Other: acute renal failure/insufficiency, retinopathy, eclampsia, microangiopathic hemolytic anemia
With the advent of antihypertensives, the incidence of hypertensive emergencies has declined from 7% to approximately 1%. In addition, the 1-year survival rate associated with this condition has increased from only 20% (prior to 1950) to more than 90% with appropriate medical treatment.
Source emedicine.com
DUC TIN SURGICAL CLINIC
Tin tức liên quan

Performance diagnostique de l’interféron gamma dans l’identification de l’origine tuberculeuse des pleurésies exsudatives

A Mixed Phenotype of Airway Wall Thickening and Emphysema Is Associated with Dyspnea and Hospitalization for Chronic Obstructive Pulmonary Disease.

Radiological Approach to Asthma and COPD-The Role of Computed Tomography.

Significant annual cost savings found with UrgoStart in UK and Germany

Thrombolex announces 510(k) clearance of Bashir catheter systems for thromboembolic disorders
Phone: (028) 3981 2678
Mobile: 0903 839 878 - 0909 384 389







