Pathophysiology
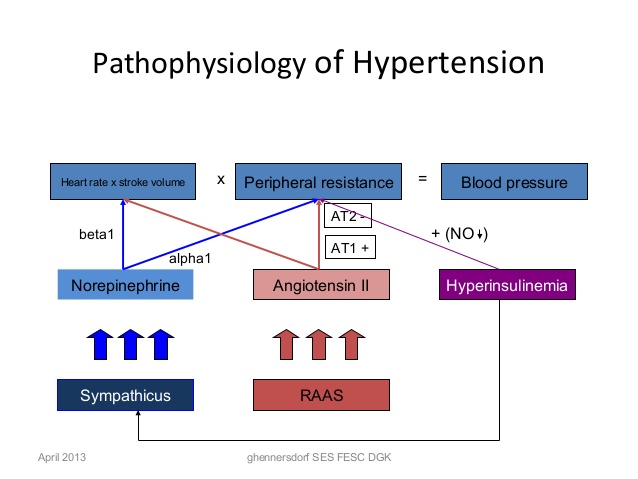
The pathogenesis of essential hypertension is multifactorial and highly complex. Multiple factors modulate the blood pressure (BP) for adequate tissue perfusion and include humoral mediators,
vascular reactivity, circulating blood volume, vascular caliber, blood viscosity, cardiac output, blood vessel elasticity, and neural stimulation. A possible pathogenesis of essential hypertension has been proposed in which multiple factors, including genetic predisposition, excess dietary salt intake, and adrenergic tone, may interact to produce hypertension. Although genetics appears to contribute to essential hypertension, the exact mechanism has not been established.
Due to investigations into the pathophysiology of hypertension, both in animals and humans, growing evidence suggests that hypertension may have an immunological basis. Studies have revealed that hypertension is associated with renal infiltration of immune cells and that pharmacologic immunosuppression (such as with the drug mycophenolate mofetil) or pathologic immunosuppression (such as occurs with HIV) results in reduced blood pressure in animals and humans. Evidence suggests that T lymphocytes and T-cell derived cytokines (eg, interleukin 17, tumor necrosis factor alpha) play an important role in hypertension.
One hypothesis is that prehypertension results in oxidation and altered mechanical forces that lead to the formation of neoantigens, which are then presented to T cells, leading to T-cell activation and infiltration of critical organs (eg, kidney, vasculature). This results in persistent or severe hypertension and end organ damage. Sympathetic nervous system activation and noradrenergic stimuli have also been shown to promote T-lymphocyte activation and infiltration and contribute to the pathophysiology of hypertension.
The natural history of essential hypertension evolves from occasional to established hypertension. After a long invariable asymptomatic period, persistent hypertension develops into complicated hypertension, in which end-organ damage to the aorta and small arteries, heart, kidneys, retina, and central nervous system is evident.
The progression of essential hypertension is as follows:
- Prehypertension in persons aged 10-30 years (by increased cardiac output)
- Early hypertension in persons aged 20-40 years (in which increased peripheral resistance is prominent)
- Established hypertension in persons aged 30-50 years
- Complicated hypertension in persons aged 40-60 years
One mechanism of hypertension has been described as high-output hypertension. High-output hypertension results from decreased peripheral vascular resistance and concomitant cardiac stimulation by adrenergic hyperactivity and altered calcium homeostasis. A second mechanism manifests with normal or reduced cardiac output and elevated systemic vascular resistance due to increased vasoreactivity. Another (and overlapping) mechanism is increased salt and water reabsorption (salt sensitivity) by the kidney, which increases circulating blood volume.
Cortisol reactivity, an index of hypothalamic-pituitary-adrenal function, may be another mechanism by which psychosocial stress is associated with future hypertension. In a prospective substudy of the Whitehall II cohort, with 3 years follow-up of an occupational cohort in previously healthy patients, investigators reported 15.9% of the patient sample developed hypertension in response to laboratory-induced mental stressors and found an association between cortisol stress reactivity and incident hypertension
Source emedicine.com
DUC TIN SURGICAL CLINIC
Tin tức liên quan

Performance diagnostique de l’interféron gamma dans l’identification de l’origine tuberculeuse des pleurésies exsudatives

A Mixed Phenotype of Airway Wall Thickening and Emphysema Is Associated with Dyspnea and Hospitalization for Chronic Obstructive Pulmonary Disease.

Radiological Approach to Asthma and COPD-The Role of Computed Tomography.

Significant annual cost savings found with UrgoStart in UK and Germany

Thrombolex announces 510(k) clearance of Bashir catheter systems for thromboembolic disorders
Phone: (028) 3981 2678
Mobile: 0903 839 878 - 0909 384 389







