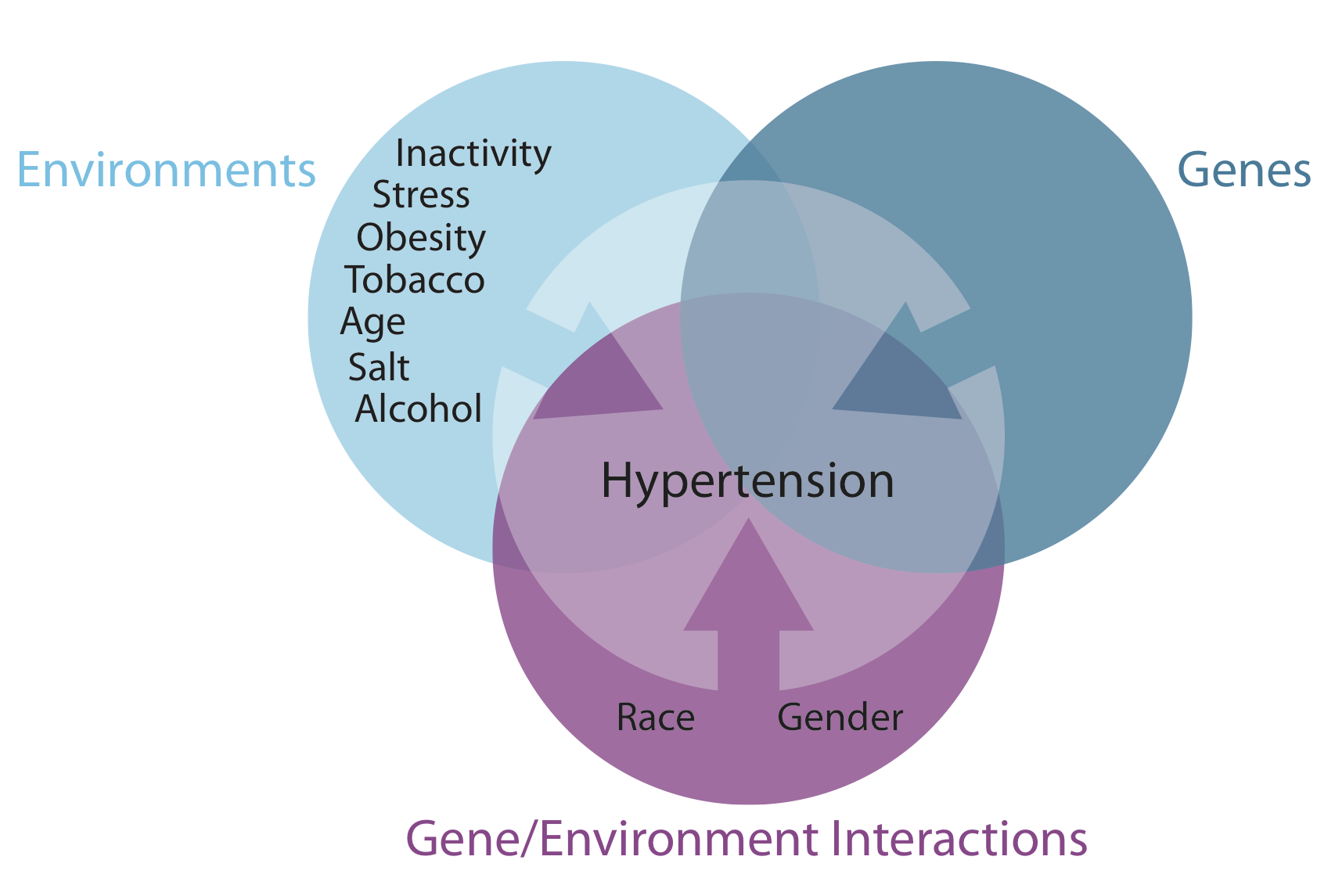
Hypertension may be primary, which may develop as a result of environmental or genetic causes, or secondary, which has multiple etiologies, including renal, vascular, and endocrine causes.
Primary or essential hypertension accounts for 90-95% of adult cases, and a small percentage of patients (2-10%) have a secondary cause. Hypertensive emergencies are most often precipitated by inadequate medication or poor compliance.
1.Environmental and genetic/epigenetic causes
Hypertension develops secondary to environmental factors, as well as multiple genes, whose inheritance appears to be complex. Furthermore, obesity, diabetes, and heart disease also have genetic components and contribute to hypertension. Epidemiological studies using twin data and data from Framingham Heart Study families reveal that BP has a substantial heritable component, ranging from 33-57%.
In an attempt to elucidate the genetic components of hypertension, multiple genome wide association studies (GWAS) have been conducted, revealing multiple gene loci in known pathways of hypertension as well as some novel genes with no known link to hypertension as of yet. Further research into these novel genes, some of which are immune-related, will likely increase the understanding of hypertension's pathophysiology, allowing for increased risk stratification and individualized treatment.
Epigenetic phenomena, such as DNA methylation and histone modification, have also been implicated in the pathogenesis of hypertension. For example, a high-salt diet appears to unmask nephron development caused by methylation. Maternal water deprivation and protein restriction during pregnancy increase renin-angiotensin expression in the fetus. Mental stress induces a DNA methylase, which enhances autonomic responsiveness. The pattern of serine protease inhibitor gene methylation predicts preeclampsia in pregnant women.
Despite these genetic findings, targeted genetic therapy seems to have little impact on hypertension. In the general population, not only does it appear that individual and joint genetic mutations have very small effects on BP levels, but it has not been shown that any of these genetic abnormalities are responsible for any applicable percentage of cases of hypertension in the general population.
Secondary causes of hypertension related to single genes are very rare. They include Liddle syndrome, glucocorticoid-remediable hyperaldosteronism, 11 beta-hydroxylase and 17 alpha-hydroxylase deficiencies, the syndrome of apparent mineralocorticoid excess, and pseudohypoaldosteronism type II.
2.Causes of secondary hypertension
Renal causes (2.5-6%) of hypertension include the renal parenchymal diseases and renal vascular diseases, as follows:
- Polycystic kidney disease
- Chronic kidney disease
- Urinary tract obstruction
- Renin-producing tumor
- Liddle syndrome
Renovascular hypertension (RVHT) causes 0.2-4% of cases. Since the seminal experiment in 1934 by Goldblatt et al, RVHT has become increasingly recognized as an important cause of clinically atypical hypertension and chronic kidney disease—the latter by virtue of renal ischemia. The coexistence of renal arterial vascular (ie, renovascular) disease and hypertension roughly defines this type of nonessential hypertension. More specific diagnoses are made retrospectively when hypertension is improved after intravascular intervention.
Vascular causes include the following:
- Coarctation of aorta
- Vasculitis
- Collagen vascular disease
Endocrine causes account for 1-2% and include exogenous or endogenous hormonal imbalances. Exogenous causes include administration of steroids. The most common form of secondary hypertension is a renal cause (although the true prevalence of hyperaldosteronism is not clear).
Another common cause is endocrine: oral contraceptive use. Activation of the renin-angiotensin-aldosterone system (RAAS) is the likely mechanism, because hepatic synthesis of angiotensinogen is induced by the estrogen component of oral contraceptives. Approximately 5% of women taking oral contraceptives may develop hypertension, which abates within 6 months after discontinuation. The risk factors for oral contraceptive–associated hypertension include mild renal disease, familial history of essential hypertension, age older than 35 years, and obesity. It would be better to group oral contraceptives and steroids with drug-induced hypertension
Exogenous administration of the other steroids used for therapeutic purposes also increases blood pressure (BP), especially in susceptible individuals, mainly by volume expansion. Nonsteroidal anti-inflammatory drugs (NSAIDs) may also have adverse effects on BP. NSAIDs block both cyclooxygenase-1 (COX-1) and COX-2 enzymes. The inhibition of COX-2 can inhibit its natriuretic effect, which, in turn, increases sodium retention. NSAIDs also inhibit the vasodilating effects of prostaglandins and the production of vasoconstricting factors—namely, endothelin-1. These effects can contribute to the induction of hypertension in a normotensive or controlled hypertensive patient.
Endogenous hormonal causes include the following:
- Primary hyperaldosteronism
- Cushing syndrome
- Pheochromocytoma
- Congenital adrenal hyperplasia
Neurogenic causes include the following:
- Brain tumor
- Bulbar poliomyelitis
- Intracranial hypertension
Drugs and toxins that cause hypertension include the following:
- Alcohol
- Cocaine
- Cyclosporine, tacrolimus
- NSAIDs
- Erythropoietin
- Adrenergic medications
- Decongestants containing ephedrine
- Herbal remedies containing licorice (including licorice root) or ephedrine (and ephedra)
- Nicotine
Other causes include the following:
- Hyperthyroidism and hypothyroidism
- Hypercalcemia
- Hyperparathyroidism
- Acromegaly
- Obstructive sleep apnea
- Pregnancy-induced hypertension
Obstructive sleep apnea (OSA) is a common but frequently undiagnosed sleep-related breathing disorder defined as an average of at least 10 apneic and hypopenic episodes per sleep hour, which leads to excessive daytime sleepiness. Multiple studies have shown OSA to be an independent risk factor for the development of essential hypertension, even after adjusting for age, gender, and degree of obesity.
Approximately half of individuals with hypertension have OSA, and approximately half with OSA have hypertension. Ambulatory BP monitoring normally reveals a "dip" in BP of at least 10% during sleep. However, if a patient is a "nondipper," the chances that the patient has OSA is increased. Nondipping is thought to be caused by frequent apneic/hypopneic episodes that end with arousals associated with marked spikes in BP that last for several seconds.
Numerous studies have shown that treatment of OSA by continuous positive airway pressure (CPAP) or position therapy lowers the awake and 24-hour blood pressure levels. Unfortunately, most cases of OSA go undiagnosed. Improved physician awareness and screening for this reversible cause of hypertension is likely to lead to great improvements in quality of life and a reduced incidence of cardiovascular complications.
Causes of hypertensive emergencies
The most common hypertensive emergency is a rapid unexplained rise in BP in a patient with chronic essential hypertension. Most patients who develop hypertensive emergencies have a history of inadequate hypertensive treatment or an abrupt discontinuation of their medications
Other causes of hypertensive emergencies include the use of recreational drugs, abrupt clonidine withdrawal, post pheochromocytoma removal, and systemic sclerosis, as well as the following:
- Renal parenchymal disease: chronic pyelonephritis, primary glomerulonephritis, tubulointerstitial nephritis (accounts for 80% of all secondary causes)
- Systemic disorders with renal involvement: systemic lupus erythematosus, systemic sclerosis, vasculitides
- Renovascular disease: atherosclerotic disease, fibromuscular dysplasia, polyarteritis nodosa
- Endocrine disease: pheochromocytoma, Cushing syndrome, primary hyperaldosteronism
- Drugs: cocaine, amphetamines, cyclosporine, clonidine (withdrawal), phencyclidine, diet pills, oral contraceptive pills
- Drug interactions: monoamine oxidase inhibitors with tricyclic antidepressants, antihistamines, or tyramine-containing food
- Central nervous system factors: CNS trauma or spinal cord disorders, such as Guillain-Barré syndrome
- Coarctation of the aorta
- Preeclampsia/eclampsia
- Postoperative hypertension
Source emedicine
DUC TIN SURGICAL CLINIC
Tin tức liên quan

Performance diagnostique de l’interféron gamma dans l’identification de l’origine tuberculeuse des pleurésies exsudatives

A Mixed Phenotype of Airway Wall Thickening and Emphysema Is Associated with Dyspnea and Hospitalization for Chronic Obstructive Pulmonary Disease.

Radiological Approach to Asthma and COPD-The Role of Computed Tomography.

Significant annual cost savings found with UrgoStart in UK and Germany

Thrombolex announces 510(k) clearance of Bashir catheter systems for thromboembolic disorders
Phone: (028) 3981 2678
Mobile: 0903 839 878 - 0909 384 389







