Overview
In the United States, 15,000 deaths per year are attributed to abdominal aortic aneurysms (AAAs). Abdominal aortic aneurysms occur most commonly in individuals between 65 and 75 years of age.
They often do not cause any symptoms and are found incidentally on physical examination or imaging examinations of the abdomen.
Since 1951, when Dubost first performed repair of an AAA with a homograft, surgery has been the mainstay of treatment. Approximately 40,000 patients undergo aneurysmorrhaphy each year. Many refinements in technique have occurred during the interval, but none as significant as the stent-graft.
In 1991, Parodi et al described a novel, less invasive technique for repairing AAAs by placing a graft from within the vessel. This technique was labor intensive and involved the customized construction of the graft for each patient by sewing the graft material to a self-expanding metal skeleton. Today, there are many devices for endovascular AAA repair approved by the US Food and Drug Administration (FDA), and numerous devices are being used in clinical investigations.
The radiologic characteristics of AAAs are demonstrated in the images below.

Radiograph shows calcification of the abdominal aorta. The left wall is clearly depicted and appears aneurysmal; however, the right wall overlies the spine. Because both walls must be calcified for a diagnosis of abdominal aortic aneurysm, lack of a clear view of the right wall makes diagnosis uncertain.
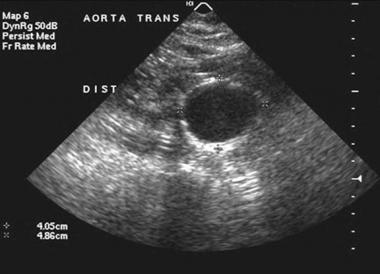
Ultrasonogram of a patient with an abdominal aortic aneurysm. This aneurysm was best visualized on a transverse or axial image. The patient underwent a conventional abdominal aortic aneurysm repair. Ultrasonography is the screening examination of choice to evaluate patients for AAA.
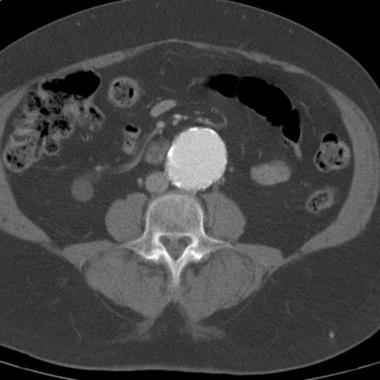
CT demonstrates an abdominal aortic aneurysm. The aneurysm was noted during workup for back pain, and CT was ordered after the abdominal aortic aneurysm was identified on radiographs. No evidence of rupture is seen.

Arteriogram demonstrates an infrarenal abdominal aortic aneurysm. This arteriogram was obtained in preparation for an endovascular repair of the aneurysm. There are coils in the right internal iliac/hypogastric artery. This was done to prevent retrograde filling of the aneurysm as the right limb of the endograft will cover the origin of the vessel.
The U.S. Preventive Services Task Force recommends a one-time screening for AAA with ultrasonography in men who are 65-75 years of age and have a history of smoking (ie, “ever smoker”: at least 100 cigarettes during lifetime). They also recommend selectively offering screening for mean 65-75 years of age who do not have a smoking history. They recommend against routine screeing in women who have never smoked and feel there is insufficient evidence to recommend screening in women who are 65-75 years of age and have a smoking history.
Preferred examination
When an examination, especially a plain radiograph, is ordered for a reason other than the evaluation of AAA, curvilinear calcifications should be carefully assessed, because most AAAs are asymptomatic. When they are discovered, the referring clinicians should be notified of the abnormal and unexpected findings. In some cases, a referring clinician might be reminded of the need for appropriate follow-up and the time interval.
Because of portability, lack of ionizing radiation, cost, and availability, ultrasonography (US) should be the initial imaging modality when an asymptomatic, pulsatile abdominal mass is palpated.
If the aneurysm is approaching 5 cm or more or if rapid enlargement is seen on serial US images, a computed tomography (CT) or CT angiography (CTA) scan should be ordered to better delineate the extent of disease prior to conventional surgery or treatment with the insertion of an endovascular graft. In patients whose renal function does not permit the administration of iodinated contrast material, magnetic resonance imaging (MRI) and magnetic resonance angiography (MRA) provide good alternatives.
Angiographic examination may be requested because of a clinical concern that concomitant renal artery stenosis or peripheral vascular disease may require surgical intervention during repair of AAAs. At some institutions, CTA and MRA have replaced routine diagnostic angiography in the preoperative evaluation of AAA.
In urgent situations in which the clinical diagnosis is fairly certain or rupture is imminent or suspected and in which the patient's condition is stable, CT and/or CTA may be the initial and only examination required.
Imaging of the aorta does not end with the repair of the aneurysm. After repair with either a traditional open surgical procedure or an endovascular procedure, follow-up imaging is necessary. In the case of conventional surgical repair, follow-up imaging is performed yearly, usually with US. For endovascular grafts, the follow-up is more stringent, with immediate postprocedural CT scanning as well as 6-month and then yearly CT scan follow-up.
When the evaluation for AAA is performed with CT or MRI, note the extent of the aneurysm, any involvement of major branch vessels, and the existence of a retroaortic or circumaortic left renal vein. Note if the aneurysm has significant wall thickening, a typical characteristic of an inflammatory aneurysm, because the surgical approach for this condition differs from that needed for the more common, predominantly atherosclerotic aneurysm.
Limitations of techniques
With conventional radiography in the anteroposterior or lateral projection, calcification of both opposing abdominal aortic walls must be present to outline AAAs. However, this finding is present in less than 50% of cases. A tortuous, calcified aorta may mimic an AAA unless both walls can be seen clearly. The lack of overlying bony structures in the lateral projection may allow clearer definition of the aneurysm.
US is considered the screening examination of choice; however, it may not adequately depict the entire abdominal aorta if a large amount of bowel gas is present or if the patient is obese.
With or without contrast enhancement, CT is an excellent screening examination for AAA. CT depicts the absolute size of the aneurysm. However, the extent of mural thrombus and the presence of dissection cannot be evaluated without the administration of contrast material. Contraindications to CTA, include anaphylactic reaction to contrast material, renal failure and pregnancy.
MRI with contrast enhancement provides an alternative to CT in patients with renal insufficiency. Contraindications to MRA, including cardiac pacemakers/AICD, electronic prosthesis, infusion pumps, certain implants and surgical clips. The use of Gd contrast is also contraindicated in patients with renal failure. Claustrophobia and a patient's inability to remain motionless are likely to yield a nondiagnostic study. MRI is not as available as CT and US.
Angiography is also a safe procedure. However, because it is an invasive procedure, a small, but definite, risk to the patient exists. The true size of the aneurysm may not be discernible because of a mural thrombus; therefore, underestimation of the true extent of the aneurysm is possible.
The role of angiography is in planning surgical or endovascular repair. For angiographic examination, CO 2 should be used as an alternative contrast in patients with renal failure. CO 2 is the only safe contrast agent in renal failure and contrast allergy. Because of buoyancy, CO 2 fills well the origins of the celiac axis and superior and inferior mesenteric arteries that arise from the ventral surface of the aorta.
Visualization of the renal artery may require elevating the side of the renal artery being examined above the injection site. CO 2 may be injected adjacent to the origin of the renal artery or selectively into the renal artery for its visualization. The common and external iliac arteries are often better visualized by reflux with the injection of CO 2 into the common femoral or external iliac artery. The catheter is advanced into the contralateral external iliac artery, and CO 2 is injected into the external or common femoral artery for visualization of the iliac arteries.
When CO 2 is trapped in the ventral portion of the AAA, the patient's body position should be changed to wash out the trapped gas. The trapped CO 2 will be rapidly replaced by less soluble blood nitrogen, which can occlude the inferior mesenteric artery (IMA), thereby stopping blood flow through the IMA and resulting in colonic ischemia.
Source emedicine.com
Duc Tin Surgical Clinic
Tin tức liên quan

Performance diagnostique de l’interféron gamma dans l’identification de l’origine tuberculeuse des pleurésies exsudatives

A Mixed Phenotype of Airway Wall Thickening and Emphysema Is Associated with Dyspnea and Hospitalization for Chronic Obstructive Pulmonary Disease.

Radiological Approach to Asthma and COPD-The Role of Computed Tomography.

Significant annual cost savings found with UrgoStart in UK and Germany

Thrombolex announces 510(k) clearance of Bashir catheter systems for thromboembolic disorders
Phone: (028) 3981 2678
Mobile: 0903 839 878 - 0909 384 389







