Myocardial infarction (MI) (ie, heart attack) is the irreversible death (necrosis) of heart muscle secondary to prolonged lack of oxygen supply (ischemia).
Approximately 1.5 million cases of MI occur annually in the United States. See the images below.
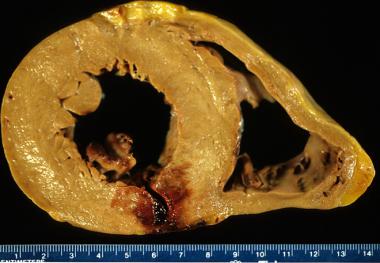
Acute myocardial infarction, reperfusion type. In this case, the infarct is diffusely hemorrhagic. There is a rupture track through the center of this posterior left ventricular transmural infarct. The mechanism of death was hemopericardium.
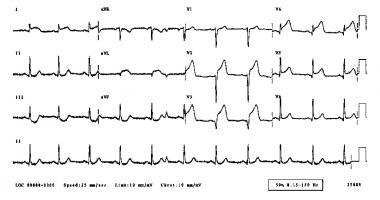
Acute anterior myocardial infarction.
Signs and symptoms
Patients with typical MI may have the following prodromal symptoms in the days preceding the event (although typical STEMI may occur suddenly, without warning):
-Fatigue
-Chest discomfort
-Malaise
Typical chest pain in acute MI has the following characteristics:
-Intense and unremitting for 30-60 minutes
-Retrosternal and often radiates up to the neck, shoulder, and jaw and down to the ulnar aspect of the left arm
-Usually described as a substernal pressure sensation that also may be characterized as squeezing, aching, burning, or even sharp
-In some patients, the symptom is epigastric, with a feeling of indigestion or of fullness and gas
The patient’s vital signs may demonstrate the following in MI:
-The patient’s heart rate is often increased secondary to a high sympathoadrenal discharge
-The pulse may be irregular because of ventricular ectopy, an accelerated idioventricular rhythm, ventricular tachycardia, atrial fibrillation or flutter, or other supraventricular arrhythmias; bradyarrhythmias may be present
-In general, the patient's blood pressure is initially elevated because of peripheral arterial vasoconstriction resulting from an adrenergic response to pain and ventricular dysfunction
-However, with right ventricular MI or severe left ventricular dysfunction, hypotension is seen
-The respiratory rate may be increased in response to pulmonary congestion or anxiety
-Coughing, wheezing, and the production of frothy sputum may occur
Diagnosis
Laboratory studies
Laboratory tests used in the diagnosis of MI include the following:
-Cardiac biomarkers/enzymes: The American College of Cardiology/American Heart Association (ACC/AHA) and the European Society of Cardiology (ESC) guidelines recommend that cardiac biomarkers should be measured at presentation in patients with suspected MI
-Troponin levels: Troponin is a contractile protein that normally is not found in serum; it is released only when myocardial necrosis occurs
-Creatine kinase (CK) levels: CK-MB levels increase within 3-12 hours of the onset of chest pain, reach peak values within 24 hours, and return to baseline after 48-72 hours
-Myoglobin levels: Myoglobin is released more rapidly from infarcted myocardium than is troponin; urine myoglobin levels rise within 1-4 hours from the onset of chest pain
-Complete blood count
-Chemistry profile
-Lipid profile
-C-reactive protein and other inflammation markers
Electrocardiography
The ECG is the most important tool in the initial evaluation and triage of patients in whom an acute coronary syndrome (ACS), such as MI, is suspected. It is confirmatory of the diagnosis in approximately 80% of cases.
Cardiac imaging
For individuals with highly probable or confirmed acute MI, coronary angiography can be used to definitively diagnose or rule out coronary artery disease.
Management
Prehospital care
For patients with chest pain, prehospital care includes the following:
-Intravenous access, supplemental oxygen, pulse oximetry
-Immediate administration of aspirin en route
-Nitroglycerin for active chest pain, given sublingually or by spray
-Telemetry and prehospital ECG, if available
Emergency department and inpatient care
Initial stabilization of patients with suspected MI and ongoing acute chest pain should include administration of sublingual nitroglycerin if patients have no contraindications to it.
The American Heart Association (AHA) recommends the initiation of beta blockers to all patients with STEMI (unless beta blockers are contraindicated).
If STEMI is present, the decision must be made quickly as to whether the patient should be treated with thrombolysis or with primary percutaneous coronary intervention (PCI).
Although patients presenting with no ST-segment elevations are not candidates for immediate administration of thrombolytic agents, they should receive anti-ischemic therapy and may be candidates for PCI urgently or during admission.
Coronary care units have reduced early mortality rates from acute MI by approximately 50% by providing immediate defibrillation and by facilitating the implementation of beneficial interventions. These interventions include the administration of intravenous (IV) medications and therapy designed to do the following:
-Limit the extent of MI
-Salvage jeopardized ischemic myocardium
-Recanalize infarct-related arteries
Source emedicine.com
Duc Tin Surgical Clinic
Tin tức liên quan

Performance diagnostique de l’interféron gamma dans l’identification de l’origine tuberculeuse des pleurésies exsudatives

A Mixed Phenotype of Airway Wall Thickening and Emphysema Is Associated with Dyspnea and Hospitalization for Chronic Obstructive Pulmonary Disease.

Radiological Approach to Asthma and COPD-The Role of Computed Tomography.

Significant annual cost savings found with UrgoStart in UK and Germany

Thrombolex announces 510(k) clearance of Bashir catheter systems for thromboembolic disorders
Phone: (028) 3981 2678
Mobile: 0903 839 878 - 0909 384 389







