Practice Essentials
Long QT syndrome is a congenital disorder characterized by a prolongation of the QT interval on electrocardiograms and a propensity to ventricular tachyarrhythmias, which may lead to syncope, cardiac arrest, or sudden death. See the image below.
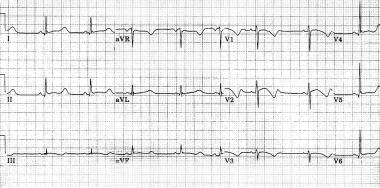
Marked prolongation of QT interval in a 15-year-old male adolescent with long QT syndrome (LQTS) (R-R = 1.00 s, QT interval = 0.56 s, QT interval corrected for heart rate [QTc] = 0.56 s). Abnormal morphology of repolarization can be observed in almost every lead (ie, peaked T waves, bowing ST segment). Bradycardia is a common feature in patients with LQTS.
Signs and symptoms
Long QT syndrome is usually diagnosed after a person has a cardiac event (eg, syncope, cardiac arrest). In some situations, this condition is diagnosed after a family member suddenly dies. In some individuals, the diagnosis is made when an electrocardiogram shows QT prolongation.
A history of cardiac events is the most typical clinical presentation in patients with LQTS.
Diagnosis
Findings on physical examination usually do not indicate a diagnosis of long QT syndrome, although some patients may present with excessive bradycardia for their age, and some patients may have hearing loss (congenital deafness), indicating the possibility of Jervell and Lange-Nielsen syndrome. Skeletal abnormalities, such as short stature and scoliosis are seen in the LQT7 type (Andersen syndrome), and congenital heart diseases, cognitive and behavioral problems, musculoskeletal diseases, and immune dysfunction may be seen in those with LQT8 type (Timothy syndrome).
Testing
Diagnostic studies in patients with suspected long QT syndrome include the following:
-Serum potassium and magnesium levels
-Thyroid function tests
-Electrocardiography of the patient and family members
-Pharmacologic provocation with epinephrine or isoproterenol in patients with a borderline presentation
-Genetic testing of the patient and family members
An increased QTc interval in response to standing up (“response to standing” test), which is associated with increased sympathetic tone, can provide more diagnostic information in patients with long QT syndrome. This increase in QTc in response to standing may persist in these patients even after heart rate returns to normal
Management
No treatment addresses the cause of long QT syndrome. Antiadrenergic therapeutic measures (eg, use of beta-blockers, left cervicothoracic stellectomy) and device therapy (eg, use of pacemakers, implantable cardioverter-defibrillators) aim to decrease the risk and lethality of cardiac events.
Pharmacotherapy
Beta-adrenergic blocking agents are the drugs of choice to treat long QT syndrome and include the following medications:
-Propranolol
-Nadolol
-Metoprolol
-Atenolol
Surgical option
Surgical intervention in patients with long QT syndrome may include the following procedures:
-Implantation of cardioverter-defibrillators
-Placement of a pacemaker
-Left cervicothoracic stellectomy
Nonpharmacotherapy
Patients with long QT syndrome should avoid participation in competitive sports, strenuous exercise, and stress-related emotions.
These individuals should also avoid the following agents:
-Anesthetics or asthma medication (eg, epinephrine)
-Antihistamines (eg, diphenhydramine; terfenadine and astemizole [both recalled from US market])
-Antibiotics (eg, erythromycin, trimethoprim and sulfamethoxazole, pentamidine)
-Cardiac medications (eg, quinidine, procainamide, disopyramide, sotalol, probucol, bepridil, dofetilide, ibutilide)
-Gastrointestinal medications (eg, cisapride)
-Antifungal medications (eg, ketoconazole, fluconazole, itraconazole)
-Psychotropic medications (eg, tricyclic antidepressants, phenothiazine derivatives, butyrophenones, benzisoxazole, diphenylbutylpiperidine)
-Potassium-loss medications (eg, indapamide, other diuretics; medications for vomiting/diarrhea)
Source emedicine.com
Duc Tin Surgical Clinic
Tin tức liên quan

Performance diagnostique de l’interféron gamma dans l’identification de l’origine tuberculeuse des pleurésies exsudatives

A Mixed Phenotype of Airway Wall Thickening and Emphysema Is Associated with Dyspnea and Hospitalization for Chronic Obstructive Pulmonary Disease.

Radiological Approach to Asthma and COPD-The Role of Computed Tomography.

Significant annual cost savings found with UrgoStart in UK and Germany

Thrombolex announces 510(k) clearance of Bashir catheter systems for thromboembolic disorders
Phone: (028) 3981 2678
Mobile: 0903 839 878 - 0909 384 389







