In 1930, Wolff, Parkinson, and White described a series of young patients who experienced paroxysms of tachycardia and had characteristic abnormalities on electrocardiography (ECG).
Currently, Wolff-Parkinson-White (WPW) syndrome is defined as a congenital condition involving abnormal conductive cardiac tissue between the atria and the ventricles that provides a pathway for a reentrant tachycardia circuit, in association with supraventricular tachycardia (SVT). See the image below for a typical "preexcited" ECG.
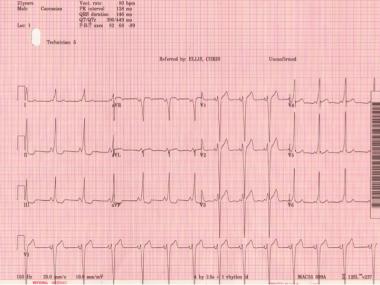
Classic Wolff-Parkinson-White electrocardiogram with short PR, QRS >120 ms, and delta wave.
Signs and symptoms
The clinical manifestations of WPW syndrome reflect the associated tachyarrhythmia episodes—rather than the anomalous ventricular excitation per se. They may have their onset at any time from childhood to middle age, and they can vary in severity from mild chest discomfort or palpitations with or without syncope to severe cardiopulmonary compromise and cardiac arrest. Thus, presentation varies by patient age.
Infants may present with the following:
- Tachypnea
- Irritability
- Pallor
- Intolerance of feedings
- Evidence of congestive heart failure if the episode has been untreated for several hours
- A history of not behaving as usual for 1-2 days
- An intercurrent febrile illness may be present
A verbal child with WPW syndrome usually reports the following:
- Chest pain
- Palpitations
- Breathing difficulty
Older patients can usually describe the following:
- Sudden onset of a pounding heartbeat
- Pulse that is regular and “too rapid to count”
- Typically, a concomitant reduction in their tolerance for activity
Physical findings include the following:
- Normal cardiac examination findings in the vast majority of cases
- During tachycardic episodes, the patient may be cool, diaphoretic, and hypotensive
- Crackles in the lungs from pulmonary vascular congestion (during or following an SVT episode)
- Many young patients may present with resting tachycardia on examination, with only minimal symptoms (eg, palpitations, weakness, mild dizziness) despite exceedingly fast heart rates
Clinical features of associated cardiac defects may be present, such as the following:
- Cardiomyopathy
- Ebstein anomaly
- Hypertrophic cardiomyopathy ( AMPK mutation)
Diagnosis
Routine blood studies may be needed to help rule out noncardiac conditions triggering tachycardia. These may include the following:
- Complete blood count
- Chemistry panel, with renal function studies and electrolytes
- Liver function tests
- Thyroid panel
- Drug screening
The diagnosis of WPW syndrome is typically made with a 12-lead electrocardiogram (ECG) and sometimes with ambulatory monitoring (eg, telemetry, Holter monitoring). SVT is best diagnosed by documenting a 12-lead ECG during tachycardia, although it is often diagnosed with a monitoring strip or even recorder. The index of suspicion is based on the history, and rarely, physical examination (Ebstein anomaly or hypertrophic cardiomyopathy [HOCM]). Although the ECG morphology varies widely, the classic ECG features are as follows:
- A shortened PR interval (typically <120 ms in a teenager or adult)
- A slurring and slow rise of the initial upstroke of the QRS complex (delta wave)
- A widened QRS complex (total duration >0.12 seconds)
- ST segment–T wave (repolarization) changes, generally directed opposite the major delta wave and QRS complex, reflecting altered depolarization
Echocardiography is needed for the following:
- Evaluation of left ventricular (LV) function, septal thickness, and wall motion abnormalities
- Excluding cardiomyopathy and an associated congenital heart defect (eg, HOCM, Ebstein anomaly, L-transposition of the great vessels)
Stress testing is ancillary and may be used for the following:
- To reproduce a transient paroxysmal SVT, which is triggered by exercise
- To document the relationship of exercise to the onset of tachycardia
- To evaluate the efficacy of antiarrhythmic drug therapy (class Ic antiarrhythmic medications and effects on antegrade preexcitation)
- To determine whether consistent or intermittent preexcitation is present at different sinus (heart) rates
Electrophysiologic studies (EPS) can be used in patients with WPW syndrome to determine the following:
- The mechanism of the clinical tachycardia
- The electrophysiologic properties (eg, conduction capability, refractory periods) of the accessory pathway and the normal atrioventricular (AV) nodal and His Purkinje conduction system
- The number and locations of accessory pathways (necessary for catheter ablation)
- The response to pharmacologic or ablation therapy
Management
Treatment of WPW associated arrhythmias comprises the following:
- Radiofrequency ablation of the accessory pathway
- Antiarrhythmic drugs to slow accessory pathway conduction
- AV nodal blocking medications in adult patients to slow AV nodal conduction in certain situations (ie, Mahaim or atriofascicular pathway-mediated SVT; typically, AV node-conduction blocking medications are avoided in the acute setting of WPW)
- For adult WPW patients, address the triggers that perpetuate the dysrhythmia, which include coronary heart disease (CAD), ischemia, cardiomyopathy, pericarditis, electrolyte disturbances, thyroid disease, and anemia
Termination of acute episodes
Narrow-complex AV reentrant tachycardia (AVRT) and AV nodal reentrant tachycardia (AVNRT) are treated by blocking AV node conduction with the following:
- Vagal maneuvers (eg, Valsalva maneuver, carotid sinus massage, splashing cold water or ice water on the face)
- Adults: IV adenosine 6-12 mg via a large-bore line (the drug has a very short half-life)
- Adults: IV verapamil 5-10 mg or diltiazem 10 mg
- Pediatric patients: Adenosine and verapamil or diltiazem are dosed on the basis of weight.
Atrial flutter/fibrillation or wide-complex tachycardia is treated as follows:
- IV procainamide or amiodarone if wide-complex tachycardia is present, ventricular tachycardia (VT) cannot be excluded, and the patient is stable hemodynamically
- Ibutilide
The initial treatment of choice for hemodynamically unstable tachycardia is direct-current synchronized electrical cardioversion, biphasic, as follows:
- A level of 100 J (monophasic or lower biphasic) initially
- If necessary, a second shock with higher energy (200 J or 360 J)
Radiofrequency ablation
Radiofrequency ablation is indicated in the following patients:
- Patients with symptomatic AVRT
- Patients with AF or other atrial tachyarrhythmias that have rapid ventricular response via an accessory pathway (preexcited AF)
- Patients with AVRT or AF with rapid ventricular rates found incidentally during EPS for unrelated dysrhythmia, if the shortest preexcited RR interval during AF is less than 250 ms
- Asymptomatic patients with ventricular preexcitation whose livelihood, profession, insurability, or mental well-being may be influenced by unpredictable tachyarrhythmias or in whom such tachyarrhythmias would endanger the public safety
- Patients with WPW and a family history of sudden cardiac death
Surgical treatment
Radiofrequency catheter ablation has virtually eliminated surgical open heart treatments in the vast majority of WPW patients, with the following exceptions:
- Patients in whom RF catheter ablation (with repeated attempts) fails
- Patients undergoing concomitant cardiac surgery (possible exception)
- Patients with other tachycardias with multiple foci who require surgical intervention (very rare)
Long-term antiarrhythmic therapy
Oral medication is the mainstay of therapy in patients not undergoing radiofrequency ablation, although the response to long-term antiarrhythmic therapy for the prevention of further episodes of tachycardia in patients with WPW syndrome remains quite variable and unpredictable. Choices include the following:
- Class Ic drugs (eg, flecainide, propafenone), typically used with an AV nodal blocking agent in low doses to avoid atrial flutter with a 1:1 conduction
- Class III drugs (eg, amiodarone, sotalol), although these are less effective for altering accessory pathway conduction properties
- In pregnancy, sotalol (class B) or flecainide (class C)
Source Emedicine.com
Duc Tin Surgery Clinic
Tin tức liên quan

Performance diagnostique de l’interféron gamma dans l’identification de l’origine tuberculeuse des pleurésies exsudatives

A Mixed Phenotype of Airway Wall Thickening and Emphysema Is Associated with Dyspnea and Hospitalization for Chronic Obstructive Pulmonary Disease.

Radiological Approach to Asthma and COPD-The Role of Computed Tomography.

Significant annual cost savings found with UrgoStart in UK and Germany

Thrombolex announces 510(k) clearance of Bashir catheter systems for thromboembolic disorders
Phone: (028) 3981 2678
Mobile: 0903 839 878 - 0909 384 389







